Noonan syndrome with multiple lentigines is caused by a different missense mutation of the same gene. Noonan syndromeis fairly common (1:1,000 to 1:2,500 live births), and neurofibromatosis 1 (which was once thought to be related to NSML) is also common (1:3500); however, no epidemiological data exists for NSML.[4]
https://en.wikipedia.org/wiki/Noonan_syndrome_with_multiple_lentigines
| Partial unilateral lentiginosis | |
|---|---|
| Other names | Segmental lentiginosis[1] |
| Specialty | Dermatology |
Partial unilateral lentiginosis is a cutaneous condition characterized by lentigines located on only one half of the body.[1]:686[2]
https://en.wikipedia.org/wiki/Partial_unilateral_lentiginosis
Peutz–Jeghers syndrome (often abbreviated PJS) is an autosomal dominant genetic disorder characterized by the development of benign hamartomatous polyps in the gastrointestinal tract and hyperpigmented macules on the lips and oral mucosa (melanosis).[1] This syndrome can be classed as one of various hereditary intestinal polyposis syndromes[2] and one of various hamartomatous polyposis syndromes.[3] It has an incidence of approximately 1 in 25,0
https://en.wikipedia.org/wiki/Peutz–Jeghers_syndrome#cite_note-4
Lentigo maligna melanoma is a melanoma that has evolved from a lentigo maligna,[1]:695 as seen as a lentigo maligna with melanoma cells invading below the boundaries of the epidermis.[2] They are usually found on chronically sun damaged skin such as the face and the forearms of the elderly.
Lentigo maligna is the non-invasive skin growth that some pathologists consider to be a melanoma-in-situ.[3] A few pathologists do not consider lentigo maligna to be a melanoma at all, but a precursor to melanomas. Once a lentigo maligna becomes a lentigo maligna melanoma, it is treated as if it were an invasive melanoma.
https://en.wikipedia.org/wiki/Lentigo_maligna_melanoma
Melanoma is a group of serious skin cancers that arise from pigment cells (melanocytes); acral lentiginous melanoma is a kind of lentiginous[6] skin melanoma.[7][8] Acral lentiginous melanoma is the most common subtype in people with darker skins and is rare in people with lighter skin types. Acral lentiginous melanoma is observed on the palms, soles, under the nails and in the oral mucosa. It occurs on non-hair-bearing surfaces of the body, which have not necessarily been exposed to sunlight. It is also found on mucous membranes.[9] It is the most common form of melanoma diagnosed amongst Asianand sub-Saharan African ethnic groups.[10] The average age at diagnosis is between sixty and se
https://en.wikipedia.org/wiki/Acral_lentiginous_melanoma
Lesions[edit]
Primary lesions[edit]
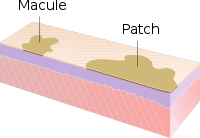
- Macule: A macule is a change in surface color, without elevation or depression and, therefore, nonpalpable, well or ill-defined,[10]variously sized, but generally considered less than either 5[10] or 10 mm in diameter at the widest point.[30]
- Patch: A patch is a large macule equal to or greater than either 5 or 10 mm across,[30] depending on one's definition of a macule.[1]Patches may have some subtle surface change, such as a fine scale or wrinkling, but although the consistency of the surface is changed, the lesion itself is not palpable.[29]
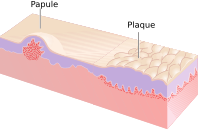
- Papule: A papule is a circumscribed, solid elevation of skin with no visible fluid, varying in size from a pinhead to less than either 5[10]or 10 mm in diameter at the widest point.[30]
- Plaque: A plaque has been described as a broad papule, or confluence of papules equal to or greater than 10 mm,[30] or alternatively as an elevated, plateau-like lesion that is greater in its diameter than in its depth.[29]
- Nodule: A nodule is morphologically similar to a papule in that it is also a palpable spherical lesion less than 10 mm in diameter. However, it is differentiated by being centered deeper in the dermis or subcutis.
- Tumour: Similar to a nodule but larger than 10 mm in diameter.[citation needed]
- Vesicle: A vesicle is small blister,[31] a circumscribed, fluid-containing, epidermal elevation generally considered less than either 5[10] or 10 mm in diameter at the widest point.[30] The fluid is clear serous fluid.[citation needed]
- Bulla: A bulla is a large blister,[31] a rounded or irregularly shaped blister containing serous or seropurulent fluid, equal to or greater than either 5[10] or 10 mm,[30] depending on one's definition of a vesicle.[1]
- Pustule: A pustule is a small elevation of the skin containing cloudy[29] or purulent material (pus) usually consisting of necrotic inflammatory cells.[30] These can be either white or red.
- Cyst: A cyst is an epithelial-lined cavity containing liquid, semi-solid, or solid material.[10]
- Wheal: A wheal is a rounded or flat-topped, pale red papule or plaque that is characteristically evanescent, disappearing within 24 to 48 hours. The temporary raised bubble of taut skin on the site of a properly-delivered intradermal injection is also called a welt, with the ID injection process itself frequently referred to as simply "raising a wheal" in medical texts.[10]
- Telangiectasia: A telangiectasia represents an enlargement of superficial blood vessels to the point of being visible.[29]
- Burrow: A burrow appears as a slightly elevated, grayish, tortuous line in the skin, and is caused by burrowing organisms.[29][30]
Secondary lesions[edit]
- Scale: dry or greasy laminated masses of keratin[30] that represent thickened stratum corneum.[29]
- Crust: dried sebum, pus, or blood usually mixed with epithelial and sometimes bacterial debris.[10]
- Lichenification: epidermal thickening characterized by visible and palpable thickening of the skin with accentuated skin markings.[1]
- Erosion: An erosion is a discontinuity of the skin exhibiting incomplete loss of the epidermis,[32] a lesion that is moist, circumscribed, and usually depressed.[21][33]
- Excoriation: a punctate or linear abrasion produced by mechanical means (often scratching), usually involving only the epidermis, but commonly reaching the papillary dermis.[30][33]
- Ulcer: An ulcer is a discontinuity of the skin exhibiting complete loss of the epidermis and often portions of the dermis and even subcutaneous fat.[32][33]
- Fissure: A fissure is a crack in the skin that is usually narrow but deep.[29][33]
- Induration: dermal thickening causing the cutaneous surface to feel thicker and firmer.[29]
- Atrophy: refers to a loss of tissue, and can be epidermal, dermal, or subcutaneous.[30] With epidermal atrophy, the skin appears thin, translucent, and wrinkled.[29] Dermal or subcutaneous atrophy is represented by depression of the skin.[29]
- Maceration: softening and turning white of the skin due to being consistently wet.
- Umbilication: formation of a depression at the top of a papule, vesicle, or pustule.[34]
- Phyma: A tubercle on any external part of the body, such as in phymatous rosacea
Configuration[edit]
"Configuration" refers to how lesions are locally grouped ("organized"), which contrasts with how they are distributed (see next section).
- Agminate: in clusters
- Annular or circinate: ring-shaped
- Arciform or arcuate: arc-shaped
- Digitate: with finger-like projections
- Discoid or nummular: round or disc-shaped
- Figurate: with a particular shape
- Guttate: resembling drops
- Gyrate: coiled or spiral-shaped
- Herpetiform: resembling herpes
- Linear
- Mammillated: with rounded, breast-like projections
- Reticular or reticulated: resembling a net
- Serpiginous: with a wavy border
- Stellate: star-shaped
- Targetoid: resembling a bullseye
- Verrucous: wart-like
Distribution[edit]
"Distribution" refers to how lesions are localized. They may be confined to a single area (a patch) or may exist in several places. Some distributions correlate with the means by which a given area becomes affected. For example, contact dermatitis correlates with locations where allergen has elicited an allergic immune response. Varicella zoster virus is known to recur (after its initial presentation as chicken pox) as herpes zoster ("shingles"). Chicken pox appears nearly everywhere on the body, but herpes zoster tends to follow one or two dermatomes; for example, the eruptions may appear along the bra line, on either or both sides of the patient.[citation needed]
- Generalized
- Symmetric: one side mirrors the other
- Flexural: on the front of the fingers
- Extensor: on the back of the fingers
- Intertriginous: in an area where two skin areas may touch or rub together
- Morbilliform: resembling measles
- Palmoplantar: on the palm of the hand or bottom of the foot
- Periorificial: around an orifice such as the mouth
- Periungual/subungual: around or under a fingernail or toenail
- Blaschkoid: following the path of Blaschko's lines in the skin
- Photodistributed: in places where sunlight reaches
- Zosteriform or dermatomal: associated with a particular nerve
[edit]
- Collarette
- Comedo
- Confluent
- Eczema (a type of dermatitis)
- Evanescent (lasting less than 24 hours)
- Granuloma
- Livedo
- Purpura
- Erythema (redness)
- Horn (a cell type)
- Poikiloderma
Histopathology[edit]
https://en.wikipedia.org/wiki/Skin_condition#Lesions
Osis - Parasite (neurocystcercosis)
tion - process/effect (formation)
ous - component/full of/presence (copious)
lysis - death/explosion/decay/deprecation/leak/swell-pull-fracture/structure def/death/dysf/rupture/etc. (lysis)
Mole - primary lesion - plaque
- Papule: A papule is a circumscribed, solid elevation of skin with no visible fluid, varying in size from a pinhead to less than either 5[10]or 10 mm in diameter at the widest point.[30]
- Plaque: A plaque has been described as a broad papule, or confluence of papules equal to or greater than 10 mm,[30] or alternatively as an elevated, plateau-like lesion that is greater in its diameter than in its depth.[29]
- Umbilication: formation of a depression at the top of a papule, vesicle, or pustule.[34]
- Phyma: A tubercle on any external part of the body, such as in phymatous rosacea
- Morbilliform: resembling measles
- Zosteriform or dermatomal: associated with a particular nerve
- For example, contact dermatitis correlates with locations where allergen has elicited an allergic immune response.
- Horn (a cell type)
- Poikiloderma
- granuloma
- scarring
- mechanism process, macro micro, wound science. trauma, surg, etc.
Freckles are clusters of concentrated melaninized cells which are most easily visible on people with a fair complexion. Freckles do not have an increased number of the melanin-producing cells, or melanocytes, but instead have melanocytes that overproduce melanin granules (melanosomes) changing the coloration of the outer skin cells (keratinocytes). As such, freckles are different from lentigines and moles,[1] which are caused by accumulation of melanocytes in a small area. Freckles can appear on all types of skin tones. Of the six Fitzpatrick skin types, they are most common on skin tones 1 and 2, which usually belong to North Europeans. However, it can be found in all ethnicities.
The presence of freckles is related to rare alleles of the MC1R gene, though it does not differentiate whether an individual will have freckles if they have one or even two copies of this gene. Also, individuals with no copies of the MC1R do sometimes display freckles. Even so, individuals with a high number of freckling sites have one or more of variants of the MC1R gene. Of the variants of the MC1R gene Arg151Cys, Arg160Trp, and Asp294His are the most common in the freckled subjects.[4][5][6] The MC1R gene is also associated with red hair more strongly than with freckles. Most red-haired individuals have two variants of the MC1R gene and almost all have one.[5] The variants that cause red hair are the same that cause freckling.[4] Freckling can also be found in areas, such as Japan, where red hair is not seen. These individuals have the variant Val92Met which is also found in white people, although it has minimal effects on their pigmentation. The R162Q allele has a disputed involvement in freckling.[7]
The variants of the MC1R gene that are linked with freckles started to emerge in the human genotype when humans started to leave Africa. The variant Val92Met arose somewhere between 250,000 and 100,000 years ago, long enough for this gene to be carried by humans into central Asia. Arg160Trp is estimated to have arisen around 80,000 years ago while Arg151Cys and Asp294His have been estimated to arise around 30,000 years ago. The wide variation of the MC1R gene exists in people of European descent because of the lack of strong environmental pressures on the gene.[8] The original allele of MC1R is coded for dark skin with a high melanin content in the cells. The high melanin content is protective in areas of high UV lightexposure.[8] The need was less as humans moved into higher altitudes where incoming sunlight has lower UV light content. The adaptation of lighter skin is needed so that individuals in higher latitudes can still absorb enough UV for the production of vitamin D.[8] Freckled individuals tend to tan less and have very light skin, which would have helped the individuals that expressed these genes absorb vitamin D.
https://en.wikipedia.org/wiki/Freckle
Mendelian traits in humans concerns how, in Mendelian inheritance, a child receiving a dominant allele from either parent will have the dominant form of the phenotypic trait or characteristic. Only those that received the recessive allele from both parents, known as zygosity, will have the recessive phenotype. Those that receive a dominant allele from one parent and a recessive allele from the other parent will have the dominant form of the trait. Purely Mendelian traits are a tiny minority of all traits, since most phenotypic traits exhibit incomplete dominance, codominance, and contributions from many genes.
The recessive phenotype may theoretically skip any number of generations, lying dormant in heterozygous "carrier" individuals until they have children with someone who also has the recessive allele and both pass it on to their child.
https://en.wikipedia.org/wiki/Mendelian_traits_in_humans
The melanocortin 1 receptor (MC1R), also known as melanocyte-stimulating hormone receptor (MSHR), melanin-activating peptide receptor, or melanotropin receptor, is a G protein–coupled receptor that binds to a class of pituitary peptide hormones known as the melanocortins, which include adrenocorticotropic hormone (ACTH) and the different forms of melanocyte-stimulating hormone (MSH). It is coupled to Gαs and upregulates levels of cAMP by activating adenylyl cyclase[5] in cells expressing this receptor. It is normally expressed in skin and melanocytes, and to a lesser degree in periaqueductal gray matter, astrocytes and leukocytes.[6] In skin cancer, MC1R is highly expressed in melanomas but not carcinomas.[7]
MC1R is one of the key proteins involved in regulating mammalian skin and hair color. It is located on the plasma membrane of specialized cells known as melanocytes, which produce the pigment melanin through the process of melanogenesis. It works by controlling the type of melanin being produced, and its activation causes the melanocyte to switch from generating the yellow or red phaeomelanin by default to the brown or black eumelanin in replacement.
MC1R has also been reported to be involved in cancer (independent of skin coloration), developmental processes, and susceptibility to infections and pain.[8]
https://en.wikipedia.org/wiki/Melanocortin_1_receptor
A lentigo (/lɛnˈtaɪɡoʊ/) (plural lentigines, /lɛnˈtɪdʒɪniːz/) is a small pigmented spot on the skin with a clearly defined edge, surrounded by normal-appearing skin. It is a harmless (benign) hyperplasia of melanocytes which is linear in its spread. This means the hyperplasia of melanocytes is restricted to the cell layer directly above the basement membrane of the epidermis where melanocytes normally reside. This is in contrast to the "nests" of multi-layer melanocytes found in moles(melanocytic nevi). Because of this characteristic feature, the adjective "lentiginous" is used to describe other skin lesions that similarly proliferate linearly within the basal cell layer.[1][2]
https://en.wikipedia.org/wiki/Lentigo
Nevus (plural nevi) is a nonspecific medical term for a visible, circumscribed, chronic lesion of the skin or mucosa.[1] The term originates from nævus, which is Latin for "birthmark"; however, a nevus can be either congenital (present at birth) or acquired. Common terms, including mole, birthmark, and beauty mark, are used to describe nevi, but these terms do not distinguish specific types of nevi from one another.
https://en.wikipedia.org/wiki/Nevus
Fibroblast, Scarring, Nevi, Melanotic, Squamous cell carcinoma, basal cell carcinoma, ageing, premature ageing, cartilage, neuro, neurodegen, cancer, atypical scarring, solar, radiation, cell cycle (integument/epidermis/etc.), lipofuscin, protein folding, proteins, fat, oxidation, oxidative stress, fat oxidation, gene, enzyme, expression, senescent, ageing, lifecycle, cell cycle arrest, timing, cell cycle metabolism, brain/neurological/brainstem, neurodegeneration/etc., metabolism (catabolic depression, anabolic function, dysequilibrium, etc.), etc..
ref. maceration, dysequ, acidbaseimb, fluids/e-, neuro-hrt-kd-lv-brn-ey-dnt, fibrosis, etc.. fungus, bacteria, decay matter, parasite, protazo amoeba, prion, nuclear infective particle, cascade, catalysis, rxn, redox, signaling, neurotransmitter, interference, receptor-enzyme-neurotransmitter-etc., osmosis, particle density, salinity, matricing of particle, matricing of sticky cell, matricing of scar, lysis scarring w dysf, HIP, nuclear particle, sporulants, tuberculosis, mites, scabies, fleas, lice, kids, bacteria, viri, virophage, bacteriophage. Particle clumping, blocking, atypicality, presence of atypical particle or dest comp, etc.. concentration, molarity, etc. (mol/L).
Immunosuppression, susceptibility to sequlae (healing rate reduction), secondary infection (presence of bacteria may require antibiotics [that do not do harm to beauty youth fertility] and to mitigate secondary infection to primary immunosuppression). Immune suppression or dysfunction may be hyper or hypo relative to estimated baseline/baseline (cannot be SD or statistical average or america norm or disease pool norm or race norm or etc.)
Not MI, ND, DEM, etc.. Dermatological conditions. No secondary.
Causes[edit]
Differently from the melanotic nevi and the verrucous nevi on the skin, age spots change in color and in shape with time. Michelitsch and Michelitsch propose a hypothesis inspired by their misrepair-accumulation aging theory[12][13] for the development of age spots.[14] They propose that aged basal cells contain lipofuscin bodies cannot be removed and might promote the aging of neighboring, generating a feedback loop whereby more and more neighbor cells become aged and lipofuscin-containing.[14] Such cells might then aggregate into a spot with an irregular shape.[14] They propose that the protruding of a flat spot is a result of the death of aged cells in the spot and release of lipofuscin bodies.[14] The aggregating cells would form a capsule, and the dense lipofuscin bodies make the protruding spot soft and dark in color.[14] However, this proposal appeared as a preprint in 2015, has little direct empirical support, and has never been published in a peer reviewed journal.
Another group[15] has reported that "age spots" taken from human skin biopsies of patients facial senile lentigo of Fitzpatrick skin type III or IV aged 55–62 are enriched with senescent fibroblasts compared to surrounding skin. The dark coloration appeared to be due to higher melanin levels and activity of tyrosinase in the senescent fibroblasts than in the controls, potentially related to lower SDF1expression.[15] Patients were then administered six weekly treatments of microneedle fractional radiofrequency aimed at eliminating dermal senescent fibroblasts; this led to a marked decrease in epidermal pigmentation compared to baseline, accompanied by a decrease in the synthesis of collagen and the normalization of suppressed SDF1 expression.[15]
https://en.wikipedia.org/wiki/Liver_spot
Liver spot
| Liver spot | |
|---|---|
 | |
| Liver spots (solar lentigo) on the left hand of a 63-year-old light-skinned Caucasian man | |
| Specialty | Dermatology Liver spots (also known as age spot, solar lentigo,[1] "lentigo senilis",[1]:686 "old age spot",[2] "senile freckle"[2]) are blemishes on the skin associated with aging[3] and exposure to ultraviolet radiation from the sun.[4] They range in color from light brown[5] to red or black and are located in areas most often exposed to the sun, particularly the hands, face, shoulders, arms and forehead, and the scalp if bald. The spots derive their name from the fact that they were once incorrectly believed to be caused by liver problems, but they are physiologically unrelated to the liver, save for a similar color.[6] From the age of 40, the skin is less able to regenerate from sun exposure, and liver spots are very common in this age group, particularly in those who spend time in the sun.[7] In the overwhelming majority of cases, liver spots pose no threat and require no treatment, though they occasionally have been known to obscure the detection of skin cancer. However, despite being a benign condition, liver spots are sometimes considered unsightly and some people choose to have them removed. This can be done by electrosurgery, laser treatment, cryotherapy, or the use of depigmentation agents, such as hydroquinone,[8] tretinoin,[8] topical cysteamine,[9] azelaic acid,[10]or alpha hydroxy acids.[11] |