| Principles of pathology |
|---|
Blog Archive
- Apr 12 (12)
- Apr 13 (2)
- Apr 14 (7)
- Apr 15 (11)
- Apr 16 (5)
- Apr 17 (14)
- Apr 18 (16)
- Apr 19 (17)
- Apr 20 (28)
- Apr 21 (29)
- Apr 22 (15)
- Apr 23 (19)
- Apr 24 (8)
- Apr 25 (58)
- Apr 26 (44)
- Apr 28 (6)
- Apr 29 (6)
- Apr 30 (7)
- May 01 (8)
- May 02 (9)
- May 03 (4)
- May 04 (6)
- May 05 (14)
- May 06 (20)
- May 07 (11)
- May 08 (18)
- May 09 (6)
- May 10 (17)
- May 11 (8)
- May 12 (25)
- May 13 (8)
- May 14 (2)
- May 15 (2)
- May 17 (16)
- May 18 (1)
- May 19 (5)
- May 20 (22)
- May 21 (6)
- May 22 (3)
- May 23 (2)
- May 24 (7)
- May 25 (1)
- May 26 (6)
- May 27 (3)
- May 28 (3)
- May 29 (10)
- May 30 (8)
- May 31 (12)
- Jun 01 (1)
- Jun 02 (1)
- Jun 03 (9)
- Jun 04 (1)
- Jun 05 (2)
- Jun 07 (4)
- Jun 08 (8)
- Jun 09 (1)
- Jun 10 (1)
- Jun 19 (1)
- Jun 27 (1)
- Jun 29 (1)
- Jun 30 (7)
- Jul 01 (3)
- Jul 02 (1)
- Jul 03 (1)
- Jul 04 (2)
- Jul 05 (1)
- Jul 06 (3)
- Jul 08 (9)
- Jul 09 (1)
- Jul 10 (1)
- Jul 11 (2)
- Jul 12 (2)
- Jul 13 (4)
- Jul 14 (4)
- Jul 15 (2)
- Jul 17 (8)
- Jul 18 (17)
- Jul 19 (1)
- Jul 20 (8)
- Jul 21 (6)
- Jul 22 (12)
- Jul 23 (10)
- Jul 25 (6)
- Jul 26 (23)
- Jul 28 (50)
- Jul 30 (12)
- Jul 31 (5)
- Aug 01 (16)
- Aug 02 (5)
- Aug 03 (5)
- Aug 04 (11)
- Aug 05 (13)
- Aug 06 (7)
- Aug 07 (10)
- Aug 08 (2)
- Aug 09 (27)
- Aug 10 (15)
- Aug 11 (67)
- Aug 12 (44)
- Aug 13 (29)
- Aug 14 (120)
- Aug 15 (61)
- Aug 16 (36)
- Aug 17 (21)
- Aug 18 (5)
- Aug 21 (5)
- Aug 22 (54)
- Aug 23 (101)
- Aug 24 (100)
- Aug 25 (99)
- Aug 26 (100)
- Aug 27 (84)
- Aug 28 (73)
- Aug 29 (76)
- Aug 30 (67)
- Aug 31 (95)
- Sep 01 (126)
- Sep 02 (68)
- Sep 03 (11)
- Sep 04 (14)
- Sep 05 (47)
- Sep 06 (101)
- Sep 07 (61)
- Sep 08 (57)
- Sep 09 (46)
- Sep 10 (14)
- Sep 11 (93)
- Sep 12 (101)
- Sep 13 (101)
- Sep 14 (100)
- Sep 15 (77)
- Sep 16 (2)
- Sep 17 (101)
- Sep 18 (91)
- Sep 19 (102)
- Sep 20 (102)
- Sep 21 (94)
- Sep 22 (84)
- Sep 23 (110)
- Sep 24 (101)
- Sep 25 (76)
- Sep 26 (43)
- Sep 27 (87)
- Sep 28 (104)
- Sep 29 (92)
- Sep 30 (33)
- Oct 01 (58)
- Oct 02 (1)
- Oct 05 (8)
- Oct 06 (6)
- Oct 07 (4)
- Oct 08 (4)
- Oct 09 (1)
- Oct 10 (18)
- Oct 11 (8)
- Oct 12 (26)
- Oct 13 (6)
- Oct 14 (2)
- Oct 15 (4)
- Oct 16 (3)
- Oct 17 (4)
- Oct 18 (3)
- Oct 19 (11)
- Oct 20 (5)
- Oct 21 (7)
- Oct 22 (5)
- Oct 23 (8)
- Oct 24 (9)
- Oct 25 (14)
- Oct 26 (8)
- Oct 27 (13)
- Oct 28 (7)
- Oct 29 (7)
- Oct 30 (22)
- Oct 31 (13)
- Nov 01 (13)
- Nov 02 (6)
- Nov 03 (10)
- Nov 04 (17)
- Nov 05 (8)
- Nov 06 (9)
- Nov 07 (11)
- Nov 08 (3)
- Nov 09 (7)
- Nov 10 (5)
- Nov 11 (5)
- Nov 12 (5)
- Nov 13 (10)
- Nov 14 (7)
- Nov 15 (15)
- Nov 16 (8)
- Nov 17 (6)
- Nov 18 (5)
- Nov 19 (7)
- Nov 20 (8)
- Nov 21 (12)
- Nov 22 (5)
- Nov 23 (7)
- Nov 24 (7)
- Nov 25 (8)
- Nov 26 (2)
- Nov 27 (12)
- Nov 28 (2)
- Nov 29 (2)
- Dec 01 (1)
- Dec 02 (3)
- Dec 03 (2)
- Dec 04 (1)
- Dec 05 (9)
- Dec 06 (22)
- Dec 07 (2)
- Dec 08 (3)
- Dec 09 (1)
- Dec 13 (2)
- Dec 14 (12)
- Dec 15 (1)
- Dec 17 (1)
- Dec 23 (4)
- Dec 24 (2)
- Dec 25 (1)
- Dec 27 (2)
- Dec 28 (1)
- Dec 29 (6)
- Dec 30 (2)
- Dec 31 (6)
- Jan 03 (3)
- Jan 04 (12)
- Jan 05 (5)
- Jan 06 (7)
- Jan 07 (1)
- Jan 08 (3)
- Jan 09 (1)
- Jan 11 (1)
- Jan 12 (5)
- Jan 14 (1)
- Jan 16 (1)
- Jan 17 (1)
- Jan 18 (2)
- Jan 23 (1)
- Jan 26 (3)
- Jan 28 (2)
- Jan 29 (3)
- Jan 30 (1)
- Jan 31 (1)
- Feb 04 (2)
- Feb 05 (2)
- Feb 08 (2)
- Feb 09 (1)
- Feb 13 (3)
- Feb 15 (2)
- Feb 16 (1)
- Feb 17 (1)
- Feb 25 (2)
- Feb 28 (2)
- Mar 03 (1)
- Mar 08 (3)
- Mar 16 (2)
- Mar 17 (1)
- Mar 18 (11)
- Mar 20 (9)
- Mar 22 (1)
- Mar 23 (3)
- Mar 31 (1)
- Apr 01 (2)
- Apr 02 (1)
- Apr 03 (2)
- Apr 04 (1)
- Apr 05 (2)
- Apr 06 (6)
- Apr 07 (1)
- Apr 08 (7)
- Apr 09 (4)
- Apr 10 (7)
- Apr 19 (18)
- Apr 20 (12)
- Apr 21 (1)
- Apr 24 (2)
- May 11 (1)
- May 16 (4)
- May 20 (2)
- May 24 (2)
- May 27 (3)
- Jun 02 (2)
- Jun 06 (1)
- Jun 07 (9)
- Jun 10 (1)
- Jun 11 (2)
- Jun 12 (3)
- Jun 15 (1)
- Jun 17 (1)
- Jun 20 (5)
- Jun 21 (12)
- Jun 22 (21)
- Jun 23 (10)
- Jun 24 (4)
- Jun 25 (10)
- Jun 26 (5)
- Jun 28 (4)
- Jun 29 (2)
- Jun 30 (2)
- Jul 01 (1)
- Jul 04 (1)
- Jul 05 (2)
- Jul 06 (1)
- Jul 07 (2)
- Jul 08 (1)
- Jul 09 (3)
- Jul 10 (6)
- Jul 11 (7)
- Jul 12 (2)
- Jul 13 (3)
- Jul 14 (7)
- Jul 15 (4)
- Jul 16 (9)
- Jul 17 (2)
- Jul 18 (6)
- Jul 19 (6)
- Jul 20 (14)
- Jul 21 (2)
- Jul 22 (6)
- Jul 23 (14)
- Jul 24 (6)
- Jul 25 (5)
- Jul 26 (5)
- Jul 27 (2)
- Jul 28 (6)
- Jul 29 (1)
- Jul 30 (3)
- Jul 31 (1)
- Aug 01 (6)
- Aug 03 (6)
- Aug 04 (4)
- Aug 05 (2)
- Aug 06 (2)
- Aug 07 (1)
- Aug 08 (1)
- Aug 09 (1)
- Aug 10 (1)
- Aug 11 (3)
- Aug 12 (1)
- Aug 13 (1)
- Aug 14 (1)
- Aug 15 (1)
- Aug 17 (9)
- Aug 19 (1)
- Aug 24 (1)
- Aug 28 (1)
- Oct 14 (1)
- Oct 22 (1)
- Nov 13 (10)
- Nov 14 (1)
- Nov 15 (3)
- Nov 23 (2)
- Nov 24 (1)
- Nov 25 (1)
- Nov 26 (1)
- Dec 01 (3)
- Dec 07 (3)
- Dec 08 (1)
- Dec 10 (2)
- Dec 12 (22)
- Dec 13 (30)
- Dec 15 (7)
- Dec 20 (5)
- Dec 28 (1)
- Dec 29 (3)
- Dec 31 (1)
- Jan 02 (2)
- Jan 10 (1)
- Jan 14 (1)
- Jan 17 (4)
- Jan 29 (2)
- Feb 03 (1)
- Feb 04 (6)
- Feb 05 (5)
- Feb 06 (10)
- Feb 08 (16)
- Feb 10 (63)
- Feb 11 (39)
- Feb 12 (33)
- Feb 13 (27)
- Feb 14 (4)
- Feb 15 (66)
- Feb 16 (7)
- Feb 17 (22)
- Feb 18 (14)
- Feb 19 (44)
- Feb 20 (3)
- Feb 21 (12)
- Feb 22 (68)
- Feb 23 (78)
- Feb 25 (3)
- Feb 26 (10)
- Feb 27 (28)
- Feb 28 (26)
- Mar 01 (17)
- Mar 02 (7)
- Mar 03 (6)
- Mar 04 (3)
- Mar 05 (7)
- Mar 06 (8)
- Mar 07 (13)
- Mar 08 (6)
- Mar 09 (3)
- Mar 10 (2)
- Mar 11 (15)
- Mar 12 (6)
- Mar 13 (2)
- Mar 14 (15)
- Mar 15 (10)
- Mar 16 (6)
- Mar 17 (5)
- Mar 18 (3)
- Mar 19 (3)
- Mar 20 (9)
- Mar 21 (2)
- Mar 22 (1)
- Mar 23 (15)
- Mar 24 (1)
- Mar 25 (1)
- Mar 26 (7)
- Mar 27 (5)
- Mar 28 (2)
- Mar 29 (8)
- Mar 30 (21)
- Mar 31 (10)
- Apr 01 (3)
- Apr 02 (3)
- Apr 03 (9)
- Apr 04 (1)
- Apr 05 (4)
- Apr 06 (4)
- Apr 07 (4)
- Apr 08 (4)
- Apr 09 (1)
- Apr 10 (1)
- Apr 11 (6)
- Apr 12 (7)
- Apr 13 (3)
- Apr 14 (2)
- Apr 15 (11)
- Apr 16 (16)
- Apr 17 (12)
- Apr 18 (29)
- Apr 19 (21)
- Apr 20 (3)
- Apr 21 (8)
- Apr 22 (3)
- Apr 23 (5)
- Apr 24 (1)
- Apr 25 (4)
- Apr 26 (6)
- Apr 27 (8)
- Apr 28 (10)
- Apr 30 (2)
- May 01 (7)
- May 02 (3)
- May 03 (16)
- May 04 (3)
- May 05 (11)
- May 06 (41)
- May 07 (2)
- May 08 (18)
- May 09 (117)
- May 10 (15)
- May 11 (85)
- May 12 (12)
- May 13 (54)
- May 14 (73)
- May 15 (85)
- May 16 (148)
- May 17 (101)
- May 18 (100)
- May 19 (99)
- May 20 (101)
- May 21 (101)
- May 22 (101)
- May 23 (101)
- May 24 (101)
- May 25 (7)
- May 27 (1)
- May 28 (1)
- May 29 (29)
- Jun 02 (1)
- Jun 03 (21)
- Jun 04 (7)
- Jun 05 (8)
- Jun 06 (1)
- Jun 22 (5)
- Jun 23 (10)
- Jun 24 (10)
- Jun 25 (4)
- Jun 26 (7)
- Jun 27 (22)
- Jun 28 (12)
- Jun 29 (11)
- Jun 30 (23)
- Jul 01 (10)
- Jul 02 (13)
- Jul 03 (17)
- Jul 04 (41)
- Jul 05 (17)
- Jul 06 (8)
- Jul 07 (10)
- Jul 08 (6)
- Jul 09 (3)
- Jul 10 (2)
- Jul 11 (2)
- Jul 12 (12)
- Jul 13 (6)
- Jul 14 (14)
- Jul 15 (5)
- Jul 17 (1)
- Jul 18 (1)
- Jul 19 (1)
- Jul 20 (1)
- Jul 22 (2)
- Jul 23 (30)
- Jul 24 (5)
- Jul 25 (55)
- Jul 27 (8)
- Jul 28 (26)
- Jul 29 (15)
- Jul 30 (35)
- Jul 31 (5)
- Aug 01 (13)
- Aug 02 (3)
- Aug 04 (1)
- Aug 05 (2)
- Aug 11 (11)
- Aug 13 (3)
- Aug 14 (7)
- Aug 15 (3)
- Aug 16 (5)
- Aug 17 (4)
- Aug 18 (4)
- Aug 19 (2)
- Aug 20 (19)
- Aug 21 (38)
- Aug 23 (14)
- Aug 24 (6)
- Aug 25 (30)
- Aug 26 (57)
- Aug 27 (19)
- Aug 28 (25)
- Aug 29 (120)
- Aug 30 (82)
- Aug 31 (46)
- Sep 01 (96)
- Sep 02 (101)
- Sep 03 (62)
- Sep 04 (32)
- Sep 05 (44)
- Sep 06 (91)
- Sep 07 (22)
- Sep 08 (100)
- Sep 09 (71)
- Sep 10 (15)
- Sep 11 (90)
- Sep 13 (2)
Wednesday, September 1, 2021
09-01-2021-1759 - Principles of pathology
09-01-2021-1756 - Liquefactive necrosis (or colliquative necrosis) Calcinosis cutis
Liquefactive necrosis (or colliquative necrosis) is a type of necrosis which results in a transformation of the tissue into a liquid viscous mass.[1]Often it is associated with focal bacterial or fungal infections, and can also manifest as one of the symptoms of an internal chemical burn.[2] In liquefactive necrosis, the affected cell is completely digested by hydrolytic enzymes, resulting in a soft, circumscribed lesion consisting of pus and the fluid remains of necrotic tissue. Dead leukocytes will remain as a creamy yellow pus.[1] After the removal of cell debris by white blood cells, a fluid filled space is left. It is generally associated with abscess formation and is commonly found in the central nervous system.
Due to excitotoxicity, hypoxic death of cells within the central nervous system can result in liquefactive necrosis.[1] This is a process in which lysosomes turn tissues into pus as a result of lysosomal release of digestive enzymes. Loss of tissue architecture means that the tissue can be liquefied. This process is not associated with bacterial action or infection. Ultimately, in a living patient most necrotic cells and their contents disappear.
The affected area is soft with liquefied centre containing necrotic debris. Later, a cyst wall is formed.
Microscopically, the cystic space contains necrotic cell debris and macrophages filled with phagocytosed material. The cyst wall is formed by proliferating capillaries, inflammatory cells, and gliosis (proliferating glial cells) in the case of brain and proliferating fibroblasts in the case of abscess cavities. Brain cells have a large amount of digestive enzymes (hydrolases). These enzymes cause the neural tissue to become soft and liquefy.
Liquefactive necrosis can also occur in the lung, especially in the context of lung abscesses.[3][4]
Liquefactive necrosis can also take place due to certain infections. Neutrophils, fighting off a bacteria, will release hydrolytic enzymes which will also attack the surrounding tissues.
https://en.wikipedia.org/wiki/Liquefactive_necrosis
Also occur in teeth and tuber etc..
Calcinosis cutis is a type of calcinosis wherein calcium deposits form in the skin. A variety of factors can result in this condition. The most common source is dystrophic calcification, which occurs in soft tissue as a response to injury. In addition, calcinosis is seen in Limited Cutaneous Systemic Sclerosis, also known as CREST syndrome (the "C" in CREST). In dogs, calcinosis cutis is found in young, large breed dogs and is thought to occur after a traumatic injury.
https://en.wikipedia.org/wiki/Calcinosis_cutis
09-01-2021-1754 - catabolism, anabolism cachexia, anorexia, pyrexia pathology caseating granuloma of tuberculosis in the adrenal gland
External links[edit]
https://en.wikipedia.org/wiki/Caseous_necrosis
catabolism, anabolism
cachexia, anorexia, pyrexia
09-01-2021-1751 - Caseous necrosis or caseous degeneration
Caseous necrosis or caseous degeneration[1] (/ˈkeɪsiəs/)[2] is a unique form of cell death in which the tissue maintains a cheese-like appearance.[3] It is also a distinctive form of coagulative necrosis.[4] The dead tissue appears as a soft and white proteinaceous dead cell mass.
Frequently, caseous necrosis is encountered in the foci of tuberculosis infections.[3] It can also be caused by syphilis and certain fungi.
A similar appearance can be associated with histoplasmosis, cryptococcosis, and coccidioidomycosis.[6]
Some data suggests that the epithelioid morphology and associated barrier function of host macrophages associated with granulomas may prevent effective immune clearance of mycobacteria.[9]
Caseous necrosis in the pleura
https://en.wikipedia.org/wiki/Caseous_necrosis
09-01-2021-1749 - Necrosis nékrōsis νέκρωσις death Emphasis on Morphological patterns
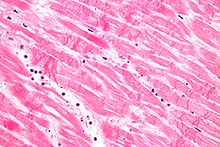
Necrosis (from Ancient Greek νέκρωσις, nékrōsis, "death") is a form of cell injury which results in the premature death of cells in living tissue by autolysis.[1] Necrosis is caused by factors external to the cell or tissue, such as infection, or trauma which result in the unregulated digestion of cell components. In contrast, apoptosis is a naturally occurring programmed and targeted cause of cellular death. While apoptosis often provides beneficial effects to the organism, necrosis is almost always detrimental and can be fatal.[2]
Morphological patterns[edit]
There are six distinctive morphological patterns of necrosis:[6]
- Coagulative necrosis is characterized by the formation of a gelatinous (gel-like) substance in dead tissues in which the architecture of the tissue is maintained,[6] and can be observed by light microscopy. Coagulation occurs as a result of protein denaturation, causing albumin to transform into a firm and opaque state.[5] This pattern of necrosis is typically seen in hypoxic (low-oxygen) environments, such as infarction. Coagulative necrosis occurs primarily in tissues such as the kidney, heart and adrenal glands.[5] Severe ischemia most commonly causes necrosis of this form.[7]
- Liquefactive necrosis (or colliquative necrosis), in contrast to coagulative necrosis, is characterized by the digestion of dead cells to form a viscous liquid mass.[6] This is typical of bacterial, or sometimes fungal, infections because of their ability to stimulate an inflammatory response. The necrotic liquid mass is frequently creamy yellow due to the presence of dead leukocytes and is commonly known as pus.[6] Hypoxicinfarcts in the brain presents as this type of necrosis, because the brain contains little connective tissue but high amounts of digestive enzymes and lipids, and cells therefore can be readily digested by their own enzymes.[5]
- Gangrenous necrosis can be considered a type of coagulative necrosis that resembles mummified tissue. It is characteristic of ischemia of lower limb and the gastrointestinal tracts. If superimposed infection of dead tissues occurs, then liquefactive necrosis ensues (wet gangrene).[8]
- Caseous necrosis can be considered a combination of coagulative and liquefactive necrosis,[5] typically caused by mycobacteria (e.g. tuberculosis), fungi and some foreign substances. The necrotic tissue appears as white and friable, like clumped cheese. Dead cells disintegrate but are not completely digested, leaving granular particles.[5] Microscopic examination shows amorphous granular debris enclosed within a distinctive inflammatory border.[6] Some granulomas contain this pattern of necrosis.[9]
- Fat necrosis is specialized necrosis of fat tissue,[9] resulting from the action of activated lipases on fatty tissues such as the pancreas. In the pancreas it leads to acute pancreatitis, a condition where the pancreatic enzymes leak out into the peritoneal cavity, and liquefy the membrane by splitting the triglyceride esters into fatty acids through fat saponification.[6] Calcium, magnesium or sodium may bind to these lesions to produce a chalky-white substance.[5] The calcium deposits are microscopically distinctive and may be large enough to be visible on radiographic examinations.[7] To the naked eye, calcium deposits appear as gritty white flecks.[7]
- Fibrinoid necrosis is a special form of necrosis usually caused by immune-mediated vascular damage. It is marked by complexes of antigenand antibodies, referred to as immune complexes deposited within arterial walls[6] together with fibrin.[6]
Other clinical classifications of necrosis[edit]
- There are also very specific forms of necrosis such as gangrene (term used in clinical practices for limbs which have suffered severe hypoxia), gummatous necrosis (due to spirochaetal infections) and hemorrhagic necrosis (due to the blockage of venous drainage of an organ or tissue).
- Some spider bites may lead to necrosis. In the United States, only spider bites from the brown recluse spider (genus Loxosceles) reliably progress to necrosis. In other countries, spiders of the same genus, such as the Chilean recluse in South America, are also known to cause necrosis. Claims that yellow sac spiders and hobo spiders possess necrotic venom have not been substantiated.
- In blind mole rats (genus Spalax), the process of necrosis replaces the role of the systematic apoptosis normally used in many organisms. Low oxygen conditions, such as those common in blind mole rats' burrows, usually cause cells to undergo apoptosis. In adaptation to higher tendency of cell death, blind mole rats evolved a mutation in the tumor suppressor protein p53 (which is also used in humans) to prevent cells from undergoing apoptosis. Human cancer patients have similar mutations, and blind mole rats were thought to be more susceptible to cancer because their cells cannot undergo apoptosis. However, after a specific amount of time (within 3 days according to a study conducted at the University of Rochester), the cells in blind mole rats release interferon-beta (which the immune system normally uses to counter viruses) in response to over-proliferation of cells caused by the suppression of apoptosis. In this case, the interferon-beta triggers cells to undergo necrosis, and this mechanism also kills cancer cells in blind mole rats. Because of tumor suppression mechanisms such as this, blind mole rats and other spalacids are resistant to cancer.[10][11]
Causes[edit]

Necrosis may occur due to external or internal factors.
External factors[edit]
External factors may involve mechanical trauma (physical damage to the body which causes cellular breakdown), damage to blood vessels (which may disrupt blood supply to associated tissue), and ischemia.[12]Thermal effects (extremely high or low temperature) can result in necrosis due to the disruption of cells.
In frostbite, crystals form, increasing the pressure of remaining tissue and fluid causing the cells to burst.[12]Under extreme conditions tissues and cells die through an unregulated process of destruction of membranes and cytosol.[13]
Internal factors[edit]
Internal factors causing necrosis include: trophoneurotic disorders (diseases that occur due to defective nerve action in a part of an organ which results in failure of nutrition); injury and paralysis of nerve cells. Pancreatic enzymes (lipases) are the major cause of fat necrosis.[12]
Necrosis can be activated by components of the immune system, such as the complement system; bacterial toxins; activated natural killer cells; and peritoneal macrophages.[1] Pathogen-induced necrosis programs in cells with immunological barriers (intestinal mucosa) may alleviate invasion of pathogens through surfaces affected by inflammation.[1] Toxins and pathogens may cause necrosis; toxins such as snake venoms may inhibit enzymes and cause cell death.[12] Necrotic wounds have also resulted from the stings of Vespa mandarinia.[14]
Pathological conditions are characterized by inadequate secretion of cytokines. Nitric oxide (NO) and reactive oxygen species (ROS) are also accompanied by intense necrotic death of cells.[12] A classic example of a necrotic condition is ischemia which leads to a drastic depletion of oxygen, glucose, and other trophic factors and induces massive necrotic death of endothelial cells and non-proliferating cells of surrounding tissues (neurons, cardiomyocytes, renal cells, etc.).[1] Recent cytological data indicates that necrotic death occurs not only during pathological events but it is also a component of some physiological process.[12]
Activation-induced death of primary T lymphocytes and other important constituents of the immune response are caspase-independent and necrotic by morphology; hence, current researchers have demonstrated that necrotic cell death can occur not only during pathological processes, but also during normal processes such as tissue renewal, embryogenesis, and immune response.[12]
Pathogenesis[edit]
Pathways[edit]
Until recently, necrosis was thought to be an unregulated process.[15] However, there are two broad pathways in which necrosis may occur in an organism.[15]
The first of these two pathways initially involves oncosis, where swelling of the cells occurs.[15] Affected cells then proceed to blebbing, and this is followed by pyknosis, in which nuclear shrinkage transpires.[15] In the final step of this pathway cell nuclei are dissolved into the cytoplasm, which is referred to as karyolysis.[15]
The second pathway is a secondary form of necrosis that is shown to occur after apoptosis and budding.[15] In these cellular changes of necrosis, the nucleus breaks into fragments (known as karyorrhexis).[15]
Histopathological changes[edit]
The nucleus changes in necrosis and characteristics of this change are determined by the manner in which its DNA breaks down:
- Karyolysis: the chromatin of the nucleus fades due to the loss of the DNA by degradation.[6]
- Karyorrhexis: the shrunken nucleus fragments to complete dispersal.[6]
- Pyknosis: the nucleus shrinks, and the chromatin condenses.[6]
Other typical cellular changes in necrosis include:
- Cytoplasmic hypereosinophilia on samples with H&E stain.[16] It is seen as a darker stain of the cytoplasm.
- The cell membrane appears discontinuous when viewed with an electron microscope. This discontinuous membrane is caused by cell blebbing and the loss of microvilli.[6]
On a larger histologic scale, pseudopalisades (false palisades) are hypercellular zones that typically surrounds necrotic tissue. Pseudopalisading necrosis indicates an aggressive tumor.[17]
Pyknosis in a bile infarct
Pseudopalisading seen around necrosis in glioblastoma.
Treatment[edit]
There are many causes of necrosis, and as such treatment is based upon how the necrosis came about. Treatment of necrosis typically involves two distinct processes: Usually, the underlying cause of the necrosis must be treated before the dead tissue itself can be dealt with.
- Debridement, referring to the removal of dead tissue by surgical or non-surgical means, is the standard therapy for necrosis. Depending on the severity of the necrosis, this may range from removal of small patches of skin to complete amputation of affected limbs or organs. Chemical removal of necrotic tissue is another option in which enzymatic debriding agents, categorised as proteolytic, fibrinolytic or collagenases, are used to target the various components of dead tissue.[18] In select cases, special maggot therapy using Lucilia sericata larvae has been employed to remove necrotic tissue and infection.[19]
- In the case of ischemia, which includes myocardial infarction, the restriction of blood supply to tissues causes hypoxia and the creation of reactive oxygen species (ROS) that react with, and damage proteins and membranes. Antioxidant treatments can be applied to scavenge the ROS.[20]
- Wounds caused by physical agents, including physical trauma and chemical burns, can be treated with antibiotics and anti-inflammatory drugs to prevent bacterial infection and inflammation. Keeping the wound clean from infection also prevents necrosis.
- Chemical and toxic agents (e.g. pharmaceutical drugs, acids, bases) react with the skin leading to skin loss and eventually necrosis. Treatment involves identification and discontinuation of the harmful agent, followed by treatment of the wound, including prevention of infection and possibly the use of immunosuppressive therapies such as anti-inflammatory drugs or immunosuppressants.[21] In the example of a snake bite, the use of anti-venom halts the spread of toxins whilst receiving antibiotics to impede infection.[22]
Even after the initial cause of the necrosis has been halted, the necrotic tissue will remain in the body. The body's immune response to apoptosis, which involves the automatic breaking down and recycling of cellular material, is not triggered by necrotic cell death due to the apoptotic pathway being disabled.[23]
In plants[edit]
If calcium is deficient, pectin cannot be synthesized, and therefore the cell walls cannot be bonded and thus an impediment of the meristems. This will lead to necrosis of stem and root tips and leaf edges.[24] For example, necrosis of tissue can occur in Arabidopsis thaliana due to plant pathogens.
Cacti such as the Saguaro and Cardon in the Sonoran Desert experience necrotic patch formation regularly; a species of Dipterans called Drosophila mettleri has developed a p450 detoxification system to enable it to use the exudates released in these patches to both nest and feed larvae.
See also[edit]
| Wikimedia Commons has media related to Necrosis. |
https://en.wikipedia.org/wiki/Necrosis