Coronavirus disease 2019 (COVID-19) is a contagious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The first known case was identified in Wuhan, China, in December 2019.[7] The disease has since spread worldwide, leading to an ongoing pandemic.[8]
Tedros Adhanom explained: CO for corona, VI for virus, D for disease and 19 for when the outbreak was first identified (31 December 2019).[32] The WHO additionally uses "the COVID-19 virus" and "the virus responsible for COVID-19" in public communications.[31]
The official names COVID-19 and SARS-CoV-2 were issued by the WHO on 11 February 2020.[31]
COVID-19 is caused by infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus strain.[52]
The respiratory route of spread of COVID-19, encompassing larger droplets and aerosols.
Infectious particles range in size from aerosols that remain suspended in the air for long periods of time to larger droplets that remain airborne or fall to the ground.[53][57] Various groups utilise terms such as "airborne" and "droplet" both in technical and general ways, leading to confusion around terminology.[58] Additionally, COVID-19 research has redefined the traditional understanding of how respiratory viruses are transmitted.[57][59] The largest droplets of respiratory fluid do not travel far, and can be inhaled or land on mucous membranes on the eyes, nose, or mouth to infect.[53] Aerosols are highest in concentration when people are in close proximity, which leads to easier viral transmission when people are physically close,[53][57][59] but airborne transmissioncan occur at longer distances, mainly in locations that are poorly ventilated;[53] in those conditions small particles can remain suspended in the air for minutes to hours.[53]
The number of people generally infected by one infected person varies;[60] as only 10 to 20% of people are responsible for the diseases spread.[61] It often spreads in clusters, where infections can be traced back to an index case or geographical location.[62]Often in these instances, superspreading events occur, where many people are infected by one person.[60]
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a novel severe acute respiratory syndrome coronavirus. It was first isolated from three people with pneumonia connected to the cluster of acute respiratory illness cases in Wuhan.[63] All structural features of the novel SARS-CoV-2 virus particle occur in related coronaviruses in nature.[64]
SARS-CoV-2 is closely related to the original SARS-CoV.[66] It is thought to have an animal (zoonotic) origin. Genetic analysis has revealed that the coronavirus genetically clusters with the genus Betacoronavirus, in subgenus Sarbecovirus (lineage B) together with two bat-derived strains. It is 96% identical at the whole genome level to other bat coronavirus samples (BatCov RaTG13).[67][68] The structural proteins of SARS-CoV-2 include membrane glycoprotein (M), envelope protein (E), nucleocapsid protein (N), and the spike protein (S). The M protein of SARS-CoV-2 is about 98% similar to the M protein of bat SARS-CoV, maintains around 98% homology with pangolin SARS-CoV, and has 90% homology with the M protein of SARS-CoV; whereas, the similarity is only around 38% with the M protein of MERS-CoV. The structure of the M protein resembles the sugar transporter SemiSWEET.[69]
The many thousands of SARS-CoV-2 variants are grouped into either clades or lineages.[70][71] The WHO, in collaboration with partners, expert networks, national authorities, institutions and researchers, have established nomenclature systems for naming and tracking SARS-CoV-2 genetic lineages by GISAID, Nextstrain and Pango. At the present time, the expert group convened by WHO has recommended the labeling of variants using letters of the Greek Alphabet, for example, Alpha, Beta, Delta, and Gamma, giving the justification that they "will be easier and more practical to discussed by non-scientific audiences."[72] Nextstrain divides the variants into five clades (19A, 19B, 20A, 20B, and 20C), while GISAID divides them into seven (L, O, V, S, G, GH, and GR).[73] The Pango tool groups variants into lineages, with many circulating lineages being classed under the B.1 lineage.[71][74]
Several notable variants of SARS-CoV-2 emerged in late 2020.[citation needed] Cluster 5 emerged among minks and mink farmers in Denmark.[citation needed] After strict quarantines and a mink euthanasia campaign, it is believed to have been eradicated.[medical citation needed]
As of July 2021, there are four dominant variants of SARS-CoV-2 spreading among global populations: the Alpha Variant (formerly called the UK Variant and officially referred to as B.1.1.7), first found in London and Kent, the Beta Variant (formerly called the South Africa Variant and officially referred to as B.1.351), the Gamma Variant (formerly called the Brazil Variant and officially referred to as P.1), and the Delta Variant (formerly called the India Variant and officially referred to as B.1.617.2).[75]
Using whole genome sequencing, epidemiology and modelling suggest the Alpha variant VUI-202012/01 (the first variant under investigation in December 2020) in the B.1.1.7 lineage transmits more easily than other strains.[76]
COVID-19 can affect the upper respiratory tract (sinuses, nose, and throat) and the lower respiratory tract (windpipe and lungs).[77] The lungs are the organs most affected by COVID-19 because the virus accesses host cells via the receptor for the enzyme angiotensin-converting enzyme 2 (ACE2), which is most abundant on the surface of type II alveolar cells of the lungs.[78] The virus uses a special surface glycoprotein called a "spike" (peplomer) to connect to the ACE2 receptor and enter the host cell.[79]
Although SARS-CoV-2 has a tropism for ACE2-expressing epithelial cells of the respiratory tract, people with severe COVID-19 have symptoms of systemic hyperinflammation. Clinical laboratory findings of elevated IL‑2, IL‑7, IL‑6, granulocyte-macrophage colony-stimulating factor (GM‑CSF), interferon gamma-induced protein 10(IP‑10), monocyte chemoattractant protein 1 (MCP1), macrophage inflammatory protein 1‑alpha (MIP‑1‑alpha), and tumour necrosis factor (TNF‑α) indicative of cytokine release syndrome (CRS) suggest an underlying immunopathology.[88]
Additionally, people with COVID-19 and acute respiratory distress syndrome (ARDS) have classical serumbiomarkers of CRS, including elevated C-reactive protein (CRP), lactate dehydrogenase (LDH), D-dimer, and ferritin.[100]
Systemic inflammation results in vasodilation, allowing inflammatory lymphocytic and monocytic infiltration of the lung and the heart. In particular, pathogenic GM-CSF-secreting T cells were shown to correlate with the recruitment of inflammatory IL-6-secreting monocytes and severe lung pathology in people with COVID-19.[101]Lymphocytic infiltrates have also been reported at autopsy.[99]
Multiple viral and host factors affect the pathogenesis of the virus. The S-protein, otherwise known as the spike protein, is the viral component that attaches to the host receptor via the ACE2 receptors. It includes two subunits: S1 and S2. S1 determines the virus-host range and cellular tropism via the receptor-binding domain. S2 mediates the membrane fusion of the virus to its potential cell host via the H1 and HR2, which are heptad repeat regions. Studies have shown that S1 domain induced IgG and IgA antibody levels at a much higher capacity. It is the focus spike proteins expression that are involved in many effective COVID-19 vaccines.[102]
The M protein is the viral protein responsible for the transmembrane transport of nutrients. It is the cause of the bud release and the formation of the viral envelope.[103] The N and E protein are accessory proteins that interfere with the host's immune response.[103]
Among healthy adults not exposed to SARS-CoV-2, about 35% have CD4+ T cells that recognize the SARS-CoV-2 S protein (particularly the S2 subunit) and about 50% react to other proteins of the virus, suggesting cross-reactivity from previous common colds caused by other coronaviruses.[106]
The severity of the inflammation can be attributed to the severity of what is known as the cytokine storm.[108]Levels of interleukin 1B, interferon-gamma, interferon-inducible protein 10, and monocyte chemoattractant protein 1 were all associated with COVID-19 disease severity. Treatment has been proposed to combat the cytokine storm as it remains to be one of the leading causes of morbidity and mortality in COVID-19 disease.[109]
A cytokine storm is due to an acute hyperinflammatory response that is responsible for clinical illness in an array of diseases but in COVID-19, it is related to worse prognosis and increased fatality. The storm causes acute respiratory distress syndrome, blood clotting events such as strokes, myocardial infarction, encephalitis, acute kidney injury, and vasculitis. The production of IL-1, IL-2, IL-6, TNF-alpha, and interferon-gamma, all crucial components of normal immune responses, inadvertently become the causes of a cytokine storm. The cells of the central nervous system, the microglia, neurons, and astrocytes, are also involved in the release of pro-inflammatory cytokines affecting the nervous system, and effects of cytokine storms toward the CNS are not uncommon.[110]
Characteristic imaging features on chest radiographs and computed tomography(CT) of people who are symptomatic include asymmetric peripheral ground-glass opacities without pleural effusions.[129]
Due to overlap with other infections such as adenovirus, imaging without confirmation by rRT-PCR is of limited specificity in identifying COVID-19.[129]
In late 2019, the WHO assigned emergency ICD-10 disease codes U07.1 for deaths from lab-confirmed SARS-CoV-2 infection and U07.2 for deaths from clinically or epidemiologically diagnosed COVID-19 without lab-confirmed SARS-CoV-2 infection.[131]
Pathology
The main pathological findings at autopsy are:
- Macroscopy: pericarditis, lung consolidation and pulmonary oedema[99]
- Lung findings:
- minor serous exudation, minor fibrin exudation[99]
- pulmonary oedema, pneumocyte hyperplasia, large atypical pneumocytes, interstitial inflammation with lymphocytic infiltration and multinucleated giant cell formation[99]
- diffuse alveolar damage (DAD) with diffuse alveolar exudates. DAD is the cause of acute respiratory distress syndrome (ARDS) and severe hypoxemia.[99]
- organisation of exudates in alveolar cavities and pulmonary interstitial fibrosis[99]
- plasmocytosis in BAL[132]
- Blood and vessels: disseminated intravascular coagulation (DIC);[133] leukoerythroblastic reaction,[134] endotheliitis,[135] hemophagocytosis[135]
- Heart: cardiac muscle cell necrosis[135]
- Liver: microvesicular steatosis[99]
- Nose: shedding of olfactory epithelium[81]
- Brain: infarction[135]
- Kidneys: acute tubular damage.[135]
- Spleen: white pulp depletion.[135]
People with more severe cases may need treatment in hospital. In those with low oxygen levels, use of the glucocorticoid dexamethasone is strongly recommended, as it can reduce the risk of death.[206][207][208] Noninvasive ventilation and, ultimately, admission to an intensive care unit for mechanical ventilation may be required to support breathing.[209] Extracorporeal membrane oxygenation (ECMO) has been used to address the issue of respiratory failure, but its benefits are still under consideration.[210][211] Some of the cases of severe disease course are caused by systemic hyper-inflammation, the so called cytokine storm.[212]
Several experimental treatments are being actively studied in clinical trials.[196] Others were thought to be promising early in the pandemic, such as hydroxychloroquine and lopinavir/ritonavir, but later research found them to be ineffective or even harmful.[196][213][214] Despite ongoing research, there is still not enough high-quality evidence to recommend so-called early treatment.[213][214] Nevertheless, in the United States, two monoclonal antibody-based therapies are available for early use in cases thought to be at high risk of progression to severe disease.[214] The antiviral remdesivir is available in the U.S., Canada, Australia, and several other countries, with varying restrictions; however, it is not recommended for people needing mechanical ventilation, and is discouraged altogether by the World Health Organization (WHO),[215] due to limited evidence of its efficacy.[196]Complications may include pneumonia, acute respiratory distress syndrome (ARDS), multi-organ failure, septic shock, and death.[249][250][251][252] Cardiovascular complications may include heart failure, arrhythmias(including atrial fibrillation), heart inflammation, and thrombosis, particularly venous thromboembolism.[253][254][255][256][257][258] Approximately 20–30% of people who present with COVID-19 have elevated liver enzymes, reflecting liver injury.[259][145]
Neurologic manifestations include seizure, stroke, encephalitis, and Guillain–Barré syndrome (which includes loss of motor functions).[260][261] Following the infection, children may develop paediatric multisystem inflammatory syndrome, which has symptoms similar to Kawasaki disease, which can be fatal.[262][263] In very rare cases, acute encephalopathy can occur, and it can be considered in those who have been diagnosed with COVID-19 and have an altered mental status.[264]
In the case of pregnant women, it is important to note that, according to the Centers for Disease Control and Prevention, pregnant women are at increased risk of becoming seriously ill from COVID-19.[265] This is because pregnant women with COVID-19 appear to be more likely to develop respiratory and obstetric complications that can lead to miscarriage, premature delivery and intrauterine growth restriction.[265]
Fungal infections such as aspergillosis, candidiasis, cryptococcosis and mucormycosis have been recorded in patients recovering from COVID-19.[266][267]
In the US, a greater proportion of deaths due to COVID-19 have occurred among African Americans and other minority groups.[315] Structural factors that prevent them from practicing social distancing include their concentration in crowded substandard housing and in "essential" occupations such as retail grocery workers, public transit employees, health-care workers and custodial staff. Greater prevalence of lacking health insurance and care of underlying conditions such as diabetes, hypertension, and heart disease also increase their risk of death.[316] Similar issues affect Native American and Latino communities.[315] On the one hand, in the Dominican Republic there is a clear example of both gender and ethnic inequality. In this Latin American territory, there is great inequality and precariousness that especially affects Dominican women, with greater emphasis on those of Haitian descent.[317] According to a US health policy non-profit, 34% of American Indian and Alaska Native People (AIAN) non-elderly adults are at risk of serious illness compared to 21% of white non-elderly adults.[318] The source attributes it to disproportionately high rates of many health conditions that may put them at higher risk as well as living conditions like lack of access to clean water.[319]
Leaders have called for efforts to research and address the disparities.[320] In the U.K., a greater proportion of deaths due to COVID-19 have occurred in those of a Black, Asian, and other ethnic minority background.[321][322][323] More severe impacts upon victims including the relative incidence of the necessity of hospitalization requirements, and vulnerability to the disease has been associated via DNA analysis to be expressed in genetic variants at chromosomal region 3, features that are associated with European Neanderthal heritage. That structure imposes greater risks that those affected will develop a more severe form of the disease.[324] The findings are from Professor Svante Pääbo and researchers he leads at the Max Planck Institute for Evolutionary Anthropology and the Karolinska Institutet.[324] This admixture of modern human and Neanderthal genes is estimated to have occurred roughly between 50,000 and 60,000 years ago in Southern Europe.[324]
The virus is thought to be natural and of an animal origin,[64] through spillover infection.[333]
Italy had its first confirmed cases on 31 January 2020, two tourists from China.[371] Italy overtook China as the country with the most deaths on 19 March 2020 .[372] By 26 March the United States had overtaken China and Italy with the highest number of confirmed cases in the world.[373] Research on coronavirus genomes indicates the majority of COVID-19 cases in New York came from European travellers, rather than directly from China or any other Asian country.[374] Retesting of prior samples found a person in France who had the virus on 27 December 2019,[375][376] and a person in the United States who died from the disease on 6 February 2020.[377]
RT-PCR testing of untreated wastewater samples from Brazil and Italy have suggested detection of SARS-CoV-2 as early as November and December 2019, respectively, but the methods of such sewage studies have not been optimised, many have not been peer-reviewed, details are often missing, and there is a risk of false positives due to contamination or if only one gene target is detected.[378] A September 2020 review journal article said, "The possibility that the COVID-19 infection had already spread to Europe at the end of last year is now indicated by abundant, even if partially circumstantial, evidence," including pneumonia case numbers and radiology in France and Italy in November and December.[379]
Humans appear to be capable of spreading the virus to some other animals, a type of disease transmission referred to as zooanthroponosis.
Some pets, especially cats and ferrets, can catch this virus from infected humans.[385][386] Symptoms in cats include respiratory (such as a cough) and digestive symptoms.[385] Cats can spread the virus to other cats, and may be able to spread the virus to humans, but cat-to-human transmission of SARS-CoV-2 has not been proven.[385][387] Compared to cats, dogs are less susceptible to this infection.[387] Behaviors which increase the risk of transmission include kissing, licking, and petting the animal.[387]
The virus does not appear to be able to infect pigs, ducks, or chickens at all.[385] Mice, rats, and rabbits, if they can be infected at all, are unlikely to be involved in spreading the virus.[387]
Tigers and lions in zoos have become infected as a result of contact with infected humans.[387] As expected, monkeys and great ape species such as orangutans can also be infected with the COVID-19 virus.[387]
Minks, which are in the same family as ferrets, have been infected.[387] Minks may be asymptomatic, and can also spread the virus to humans.[387]Multiple countries have identified infected animals in mink farms.[388] Denmark, a major producer of mink pelts, ordered the slaughter of all minks over fears of viral mutations.[388] A vaccine for mink and other animals is being researched.[388]
International research on vaccines and medicines in COVID-19 is underway by government organisations, academic groups, and industry researchers.[389][390] The CDC has classified it to require a BSL3 grade laboratory.[391] There has been a great deal of COVID-19 research, involving accelerated research processes and publishing shortcuts to meet the global demand.[392]
Repurposed antiviral drugs make up most of the research into COVID-19 treatments.[407][408] Other candidates in trials include vasodilators, corticosteroids, immune therapies, lipoic acid, bevacizumab, and recombinantangiotensin-converting enzyme 2.[408]
In March 2020, the World Health Organization (WHO) initiated the Solidarity trial to assess the treatment effects of some promising drugs: an experimental drug called remdesivir; anti-malarial drugs chloroquine and hydroxychloroquine; two anti-HIV drugs, lopinavir/ritonavir; and interferon-beta.[409][410] More than 300 active clinical trials are underway as of April 2020.[145]
Research on the antimalarial drugs hydroxychloroquine and chloroquine showed that they were ineffective at best,[411][412] and that they may reduce the antiviral activity of remdesivir.[413] By May 2020, France, Italy, and Belgium had banned the use of hydroxychloroquine as a COVID-19 treatment.[414]
A cytokine storm can be a complication in the later stages of severe COVID-19. A cytokine storm is a potentially deadly immune reaction where a large amount of pro-inflammatory cytokines and chemokines are released too quickly; A cytokine storm can lead to ARDS and multiple organ failure.[427] Data collected from Jin Yin-tan Hospital in Wuhan, China indicates that patients who had more severe responses to COVID-19 had greater amounts of pro-inflammatory cytokines and chemokines in their system than patients who had milder responses; These high levels of pro-inflammatory cytokines and chemokines indicate presence of a cytokine storm.[428]
Tocilizumab has been included in treatment guidelines by China's National Health Commission after a small study was completed.[429][430] It is undergoing a Phase II non-randomised trial at the national level in Italy after showing positive results in people with severe disease.[431][432] Combined with a serum ferritin blood test to identify a cytokine storm (also called cytokine storm syndrome, not to be confused with cytokine release syndrome), it is meant to counter such developments, which are thought to be the cause of death in some affected people.[433] The interleukin-6 receptor antagonist was approved by the FDA to undergo a Phase III clinical trial assessing its effectiveness on COVID-19 based on retrospective case studies for the treatment of steroid-refractory cytokine release syndrome induced by a different cause, CAR T cell therapy, in 2017.[434] There is no randomised, controlled evidence that tocilizumab is an efficacious treatment for CRS. Prophylactic tocilizumab has been shown to increase serum IL-6 levels by saturating the IL-6R, driving IL-6 across the blood-brain barrier, and exacerbating neurotoxicity while having no effect on the incidence of CRS.[435]
Lenzilumab, an anti-GM-CSF monoclonal antibody, is protective in murine models for CAR T cell-induced CRS and neurotoxicity and is a viable therapeutic option due to the observed increase of pathogenic GM-CSF secreting T cells in hospitalised patients with COVID-19.[436]
Transferring purified and concentrated antibodies produced by the immune systems of those who have recovered from COVID-19 to people who need them is being investigated as a non-vaccine method of passive immunisation.[437][438] Viral neutralization is the anticipated mechanism of action by which passive antibody therapy can mediate defence against SARS-CoV-2. The spike protein of SARS-CoV-2 is the primary target for neutralizing antibodies.[439] As of 8 August 2020, eight neutralizing antibodies targeting the spike protein of SARS-CoV-2 have entered clinical studies.[440] It has been proposed that selection of broad-neutralizing antibodies against SARS-CoV-2 and SARS-CoV might be useful for treating not only COVID-19 but also future SARS-related CoV infections.[439] Other mechanisms, however, such as antibody-dependent cellular cytotoxicityor phagocytosis, may be possible.[437] Other forms of passive antibody therapy, for example, using manufactured monoclonal antibodies, are in development.[437]
The use of passive antibodies to treat people with active COVID-19 is also being studied. This involves the production of convalescent serum, which consists of the liquid portion of the blood from people who recovered from the infection and contains antibodies specific to this virus, which is then administered to active patients.[437] This strategy was tried for SARS with inconclusive results.[437] An updated Cochrane review in May 2021 found high certainty evidence that for the treatment of people with moderate to severe COVID-19 convalescent plasma did not reduce mortality or bring about symptom improvement[438] There continues to be uncertainty about the safety of convalescent plasma administration to people with COVID-19 and differing outcomes measured in different studies limits their use in determining efficacy.[438]
Multisystem inflammatory syndrome in children (MIS-C), or paediatric inflammatory multisystem syndrome (PIMS / PIMS-TS), or systemic inflammatory syndrome in COVID19 (SISCoV), is a rare systemic illness involving persistent fever and extreme inflammation following exposure to SARS-CoV-2, the virus responsible for COVID-19.[7] It can rapidly lead to medical emergencies such as insufficient blood flow around the body (a condition known as shock).[7] Failure of one or more organs can occur.[8] A warning sign is unexplained persistent fever with severe symptoms following exposure to COVID-19.[9]Prompt referral to paediatric specialists is essential, and families need to seek urgent medical assistance.[7] Most affected children will need intensive care.[7]
https://en.wikipedia.org/wiki/Multisystem_inflammatory_syndrome_in_children
| Coronavirus disease 2019 (COVID-19) | |
|---|---|
| Other names | COVID, (the) coronavirus |
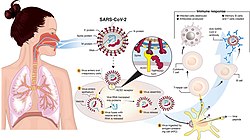 | |
Transmission and life-cycle of SARS-CoV-2causing COVID-19. | |
| Pronunciation | |
| Specialty | Infectious disease |
| Symptoms | Fever, cough, fatigue, shortness of breath, vomiting, loss of taste or smell; some cases asymptomatic[2][3] |
| Complications | Pneumonia, viral sepsis, acute respiratory distress syndrome, kidney failure, cytokine release syndrome, respiratory failure, pulmonary fibrosis, pediatric multisystem inflammatory syndrome, chronic COVID syndrome |
| Usual onset | 2–14 days (typically 5) from infection |
| Duration | 5 days to chronic |
| Causes | Severe acute respiratory syndrome coronavirus 2(SARS-CoV-2) |
| Diagnostic method | rRT-PCR testing, CT scan, Rapid antigen test |
| Prevention | Face coverings, quarantine, physical/social distancing, ventilation, hand washing,[4][needs update]vaccination[5] |
| Treatment | Symptomatic and supportive |
| Frequency | 204,440,061[6] confirmed cases |
| Deaths | 4,320,736[6] |
https://en.wikipedia.org/wiki/COVID-19
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), has many variants; some are believed, or have been believed, to be of particular importance due to their potential for increased transmissibility,[1] increased virulence, or reduced effectiveness of vaccines against them.[2][3]
https://en.wikipedia.org/wiki/Variants_of_SARS-CoV-2
Middle East respiratory syndrome (MERS), also known as camel flu,[1] is a viral respiratory infection caused by Middle East respiratory syndrome–related coronavirus (MERS-CoV).[2]Symptoms may range from none, to mild, to severe.[7][2] Typical symptoms include fever, cough, diarrhea, and shortness of breath.[2] The disease is typically more severe in those with other health problems.[2][7]
MERS-CoV is a coronavirus believed to be originally from bats.[2] However, humans are typically infected from camels, either during direct contact or indirectly.[2] Spread between humans typically requires close contact with an infected person.[2] Its spread is uncommon outside of hospitals.[7]Thus, its risk to the global population is currently deemed to be fairly low.[7] Diagnosis is by rRT-PCR testing of blood and respiratory samples.[5]
https://en.wikipedia.org/wiki/Middle_East_respiratory_syndrome
Spillover infection, also known as pathogen spillover and spillover event, occurs when a reservoir population with a high pathogen prevalence comes into contact with a novel host population. The pathogen is transmitted from the reservoir population and may or may not be transmitted within the host population.[1]
https://en.wikipedia.org/wiki/Spillover_infection
A pleural effusion is accumulation of excessive fluid in the pleural space, the potential space that surrounds each lung. Under normal conditions, pleural fluid is secreted by the parietal pleuralcapillaries at a rate of 0.01 millilitre per kilogram weight per hour, and is cleared by lymphaticabsorption leaving behind only 5–15 millilitres of fluid, which helps to maintain a functional vacuumbetween the parietal and visceral pleurae. Excess fluid within the pleural space can impair inspiration by upsetting the functional vacuum and hydrostatically increasing the resistance against lung expansion, resulting in a fully or partially collapsed lung.
Various kinds of fluid can accumulate in the pleural space, such as serous fluid (hydrothorax), blood(hemothorax), pus (pyothorax, more commonly known as pleural empyema), chyle (chylothorax), or very rarely urine (urinothorax). When unspecified, the term "pleural effusion" normally refers to hydrothorax. A pleural effusion can also be compounded by a pneumothorax (accumulation of air in the pleural space), leading to a hydropneumothorax.
https://en.wikipedia.org/wiki/Pleural_effusion
No comments:
Post a Comment