Human monocytotropic ehrlichiosis[1] is a form of ehrlichiosis associated with Ehrlichia chaffeensis.[2] This bacterium is an obligate intracellular pathogen affecting monocytes and macrophages.
| Human monocytic ehrlichiosis | |
|---|---|
 | |
| Ehrlichia chaffeensis | |
| Specialty | Infectious disease |
https://en.wikipedia.org/wiki/Human_monocytotropic_ehrlichiosis
Monocytes are a type of leukocyte, or white blood cell. They are the largest type of leukocyte and can differentiate into macrophages and conventional dendritic cells. As a part of the vertebrate innate immune system monocytes also influence the process of adaptive immunity. There are at least three subclasses of monocytes in humanblood based on their phenotypic receptors.
| Monocyte | |
|---|---|
 | |
| Details | |
| System | Immune system |
| Identifiers | |
| MeSH | D009000 |
| TH | H2.00.04.1.02010 |
| FMA | 62864 |
| Anatomical terms of microanatomy | |
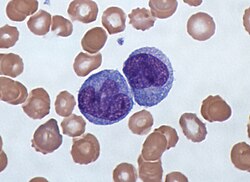
Monocytes are amoeboid in appearance, and have nongranulated cytoplasm.[1] Thus they are classified as agranulocytes. Containing unilobar nuclei, these cells are one of the types of mononuclear leukocytes which shelter azurophil granules. The archetypal geometry of the monocyte nucleus is ellipsoidal; metaphorically bean-shaped or kidney-shaped, although the most significant distinction is that the nuclear envelope should not be hyperbolically furcated into lobes. Contrast to this classification occurs in polymorphonuclear leukocytes. Monocytes compose 2% to 10% of all leukocytes in the human body and serve multiple roles in immune function. Such roles include: replenishing resident macrophages under normal conditions; migration within approximately 8–12 hours in response to inflammation signals from sites of infection in the tissues; and differentiationinto macrophages or dendritic cells to effect an immune response. In an adult human, half of the monocytes are stored in the spleen.[2] These change into macrophages after entering into appropriate tissue spaces, and can transform into foam cells in the endothelium.
Subpopulations[edit]
In humans[edit]
There are at least three types of monocytes in human blood:[3]
- The classical monocyte is characterized by high level expression of the CD14 cell surface receptor (CD14++ CD16−monocyte)
- The non-classical monocyte shows low level expression of CD14 and additional co-expression of the CD16 receptor (CD14+CD16++ monocyte).[4]
- The intermediate monocyte with high level expression of CD14 and low level expression of CD16 (CD14++CD16+monocytes).
While in humans the level of CD14 expression can be used to differentiate non-classical and intermediate monocytes, the slan (6-Sulfo LacNAc) cell surface marker was shown to give an unequivocal separation of the two cell types.[5][6]
Ghattas et al. state that the "intermediate" monocyte population is likely to be a unique subpopulation of monocytes, as opposed to a developmental step, due to their comparatively high expression of surface receptors involved in reparative processes (including vascular endothelial growth factor receptors type 1 and 2, CXCR4, and Tie-2) as well as evidence that the "intermediate" subset is specifically enriched in the bone marrow.[7] After stimulation with microbial products the CD14+CD16++ monocytes produce high amounts of pro-inflammatory cytokines like tumor necrosis factor and interleukin-12.
Said et al. showed that activated monocytes express high levels of PD-1 which might explain the higher expression of PD-1 in CD14+CD16++ monocytes as compared to CD14++CD16− monocytes. Triggering monocytes-expressed PD-1 by its ligand PD-L1 induces IL-10 production which activates CD4 Th2 cells and inhibits CD4 Th1 cell function.[8]
In humans a monocyte crawling behavior, similar to the patrolling in mice, has been demonstrated both for the classical and the non-classical monocytes.[9][clarification needed]
https://en.wikipedia.org/wiki/Monocyte
No comments:
Post a Comment