Dermatomyositis (DM) is a long-term inflammatory disorder which affects skin and the muscles.[1] Its symptoms are generally a skin rash and worsening muscle weakness over time.[1] These may occur suddenly or develop over months.[1] Other symptoms may include weight loss, fever, lung inflammation, or light sensitivity.[1] Complications may include calcium deposits in muscles or skin.[1]
The cause is unknown.[1] Theories include that it is an autoimmune disease or a result of a viral infection.[1] It is a type of inflammatory myopathy.[1]Diagnosis is typically based on some combination of symptoms, blood tests, electromyography, and muscle biopsies.[3]
While no cure for the condition is known, treatments generally improve symptoms.[1] Treatments may include medication, physical therapy, exercise, heat therapy, orthotics and assistive devices, and rest.[1] Medications in the corticosteroids family are typically used with other agents such as methotrexate or azathioprine recommended if steroids are not working well.[1]Intravenous immunoglobulin may also improve outcomes.[1] Most people improve with treatment and in some, the condition resolves completely.[1]
About one per 100,000 people per year are newly affected.[3] The condition usually occurs in those in their 40s and 50s with women being affected more often than men.[3] People of any age, however, may be affected.[3] The condition was first described in the 1800s.[4]
The diagnosis of dermatomyositis is based on five criteria, which are also used to differentially diagnose with respect to polymyositis:[7]
- Muscle weakness in both thighs or both upper arms
- Using a blood test, finding higher levels of enzymes found in skeletal muscle, including creatinine kinase, aldolase, and glutamate oxaloacetate, pyruvate transaminases and lactate dehydrogenase
- Using testing of electric signalling in muscles, finding all three of: erratic, repetitive, high-frequency signals; short, low-energy signals between skeletal muscles and motor neurons that have multiple phases; and sharp activity when a needle is inserted into the muscle
- Examining a muscle biopsy under a microscope and finding mononuclear white blood cells between the muscle cells, and finding abnormal muscle cell degeneration and regeneration, dying muscle cells, and muscle cells being consumed by other cells (phagocytosis)
- Rashes typical of dermatomyositis, which include heliotrope rash, Gottron sign, and Gottron papules
https://en.wikipedia.org/wiki/Dermatomyositis
Azathioprine (AZA), sold under the brand name Imuran, among others, is an immunosuppressive medication.[2] It is used in rheumatoid arthritis, granulomatosis with polyangiitis, Crohn's disease, ulcerative colitis, and systemic lupus erythematosus, and in kidney transplants to prevent rejection.[2][3][4][5] It is taken by mouth or injected into a vein.[2]
Common side effects include bone-marrow suppression and vomiting.[2] Bone-marrow suppression is especially common in people with a genetic deficiency of the enzyme thiopurine S-methyltransferase.[2] Other serious risk factors include an increased risk of certain cancers.[2] Use during pregnancy may result in harm to the baby.[2] Azathioprine is in the purine analogue and antimetabolite family of medications.[2][6] It works via 6-thioguanine to disrupt the making of RNA and DNA by cells.[2][6]
Azathioprine was first made in 1957.[6] It is on the World Health Organization's List of Essential Medicines.[7] In 2017, it was the 335th-most commonly prescribed medication in the United States, with more than 800,000 prescriptions.[8]

Azathioprine is listed as a human carcinogen in the 12th Report on Carcinogens by the National Toxicology Program of U.S. Department of Health and Human Services, asserting that it is "known to be a human carcinogen based on sufficient evidence of carcinogenicity from studies in humans."[43] Since August 2009, the U.S. FDA has required warnings to be placed on packaging with respect to increased risks of certain cancers.[44]
The risks involved seem to be related both to the duration and the dosage used. People who have previously been treated with an alkylating agent may have an excessive risk of cancers if treated with azathioprine. Epidemiological studies by International Agency for Research on Cancer have provided "sufficient" evidence of azathioprine carcinogenicity in humans (group 1),[45]although the methodology of past studies and the possible underlying mechanisms are questioned.[46]
The various diseases requiring transplantation may in themselves increase the risks of non-Hodgkin lymphoma, squamous cell carcinomas of the skin, hepatobiliary carcinomas, and mesenchymal tumours to which azathioprine may add additional risks. Those receiving azathioprine for rheumatoid arthritis may have a lower risk than those undergoing transplantation.[32]
Cases of hepatosplenic T-cell lymphoma – a rare type of lymphoma – have been reported in patients treated with azathioprine. The majority occurred in patients with inflammatory bowel disease. Adolescents and young adult males were the majority of cases.[47]They presented with a very aggressive disease course, and with one exception, died of the lymphoma. The FDA has required changes to the labeling to inform users and clinicians of the issue.[48]
https://en.wikipedia.org/wiki/Azathioprine
Saturday, September 11, 2021
09-10-2021-2212 - vasculitis Vasculitis Lymphangitis Lymphangitis phlebitis arteritis reticularis gangrene syphilitic aortitis cancotics dysplasia proliferative granulomateous disseminative reaction syphalli level one Civilian level one CL1 immune vasculitides haploinsufficiency of A20 genetics Eosinophilic granulomatosis with polyangiitis granulomatosis with polyangiitis, Henoch–Schönlein purpura vasiculitis vesiculitis vesculitis
Vasculitis is a group of disorders that destroy blood vessels by inflammation.[2] Both arteries and veins are affected. Lymphangitis(inflammation of lymphatic vessels) is sometimes considered a type of vasculitis.[3] Vasculitis is primarily caused by leukocyte migration and resultant damage. Although both occur in vasculitis, inflammation of veins (phlebitis) or arteries (arteritis) on their own are separate entities.
| Vasculitis | |
|---|---|
| Other names | Vasculitides[1] |
 | |
| Petechia and purpura on the lower limb due to medication-induced vasculitis. | |
Signs and symptoms[edit]
Possible signs and symptoms include:[4]
- General symptoms: Fever, unintentional weight loss
- Skin: Palpable purpura, livedo reticularis
- Muscles and joints: Muscle pain or inflammation, joint pain or joint swelling
- Nervous system: Mononeuritis multiplex, headache, stroke, tinnitus, reduced visual acuity, acute visual loss
- Heart and arteries: Heart attack, high blood pressure, gangrene
- Respiratory tract: Nose bleeds, bloody cough, lung infiltrates
- GI tract: Abdominal pain, bloody stool, perforations (hole in the GI tract)
- Kidneys: Inflammation of the kidney's filtration units (glomeruli)
Cause[edit]
Classification[edit]
Vasculitis can be classified by the cause, the location, the type of vessel or the size of vessel.
- Underlying cause. For example, the cause of syphilitic aortitis is infectious (aortitis simply refers to inflammation of the aorta, which is an artery.) However, the causes of many forms of vasculitis are poorly understood. There is usually an immune component, but the trigger is often not identified. In these cases, the antibody found is sometimes used in classification, as in ANCA-associated vasculitides. Clinical studies with immunosuppressive drugs targeting specific cytokines and cells can also be used to understand the heterogeneous immunopathogenic mechanisms of vasculitis and support a mechanistic immunological classification.[5]
- Location of the affected vessels. For example, ICD-10 classifies "vasculitis limited to skin" with skin conditions (under "L"), and "necrotizing vasculopathies" (corresponding to systemic vasculitis) with musculoskeletal system and connective tissue conditions (under "M"). Arteritis/phlebitis on their own are classified with circulatory conditions (under "I").
- Type or size of the blood vessels that they predominantly affect.[6] Apart from the arteritis/phlebitis distinction mentioned above, vasculitis is often classified by the caliber of the vessel affected. However, there can be some variation in the size of the vessels affected.
A small number have been shown to have a genetic basis. These include adenosine deaminase 2 deficiency and haploinsufficiency of A20.
According to the size of the vessel affected, vasculitis can be classified into:[7][8]
- Large vessel: Takayasu's arteritis, Temporal arteritis
- Medium vessel: Buerger's disease, Kawasaki disease, Polyarteritis nodosa
- Small vessel: Behçet's syndrome, Eosinophilic granulomatosis with polyangiitis, Cutaneous vasculitis, granulomatosis with polyangiitis, Henoch–Schönlein purpura, and microscopic polyangiitis. Condition of some disorders have vasculitis as their main feature. The major types are given in the table below:
| Comparison of major types of vasculitis | ||
|---|---|---|
| Vasculitis | Affected organs | Histopathology |
| Cutaneous small-vessel vasculitis | Skin, kidneys | Neutrophils, fibrinoid necrosis |
| Granulomatosis with polyangiitis | Nose, lungs, kidneys | Neutrophils, giant cells |
| Eosinophilic granulomatosis with polyangiitis | Lungs, kidneys, heart, skin | Histiocytes, eosinophils |
| Behçet's disease | Commonly sinuses, brain, eyes and skin; can affect other organs such as lungs, kidneys, joints | Lymphocytes, macrophages, neutrophils |
| Kawasaki disease | Skin, heart, mouth, eyes | Lymphocytes, endothelialnecrosis |
| Buerger's disease | Leg arteries and veins (gangrene) | Neutrophils, granulomas |
| "Limited" granulomatosis with polyangiitis vasculitis | Commonly sinuses, brain, and skin; can affect other organs such as lungs, kidneys, joints; | |
Takayasu's arteritis, polyarteritis nodosa and giant cell arteritis mainly involve arteries and are thus sometimes classed specifically under arteritis.
Furthermore, there are many conditions that have vasculitis as an accompanying or atypical feature, including:
- Rheumatic diseases, such as rheumatoid arthritis, systemic lupus erythematosus, and dermatomyositis
- Cancer, such as lymphomas
- Infections, such as hepatitis C
- Exposure to chemicals and drugs, such as amphetamines, cocaine, and anthrax vaccines which contain the Anthrax Protective Antigen as the primary ingredient.
In pediatric patients varicella inflammation may be followed by vasculitis of intracranial vessels. This condition is called post varicella angiopathy and this may be responsible for arterial ischaemic strokes in children.[9]
Several of these vasculitides are associated with antineutrophil cytoplasmic antibodies.[10] These are:
- Granulomatosis with polyangiitis
- Eosinophilic granulomatosis with polyangiitis
- Microscopic polyangiitis
https://en.wikipedia.org/wiki/Vasculitis
Syphilitic aortitis is inflammation of the aorta associated with the tertiary stage of syphilis infection. SA begins as inflammation of the outermost layer of the blood vessel, including the blood vessels that supply the aorta itself with blood, the vasa vasorum.[3] As SA worsens, the vasa vasorum undergo hyperplastic thickening of their walls thereby restricting blood flow and causing ischemia of the outer two-thirds of the aortic wall. Starved for oxygen and nutrients, elastic fibers become patchy and smooth muscle cells die. If the disease progresses, syphilitic aortitis leads to an aortic aneurysm. Overall, tertiary syphilis is a rare cause of aortic aneurysms.[3] Syphilitic aortitis has become rare in the developed world with the advent of penicillin treatments after World War II.[citation needed]
| Syphilitic aortitis | |
|---|---|
| Other names | SA |
 | |
| Aneurysm,a common complication of SA | |
| Specialty | Cardiology, Infectious disease |
| Symptoms | Often none |
| Complications | Aneurysm |
| Usual onset | 40-55 years old, (initial infection is generally earlier in life)[1] |
| Causes | Treponema pallidum |
| Risk factors | Unprotected sex, HIV, Drug use[2] |
| Prevention | Condoms,avoinding drug use |
https://en.wikipedia.org/wiki/Syphilitic_aortitis
Agranulocytes or nongranulocytes, also mononuclear leukocytes, are one of the two types of white blood cells, also known as leukocytes. The other type of white blood cells are known as granulocytes. Agranular cells are noted by the absence of granules in their cytoplasm, which distinguishes them from granulocytes. The two types of agranulocytes in the blood circulation are lymphocytes and monocytes, and these make up about 35% of the hematologic blood values.[1]
https://en.wikipedia.org/wiki/Agranulocyte
https://en.wikipedia.org/wiki/Mesenchyme
https://en.wikipedia.org/wiki/Cholangiocarcinoma
https://en.wikipedia.org/wiki/Hepatosplenic_T-cell_lymphoma
https://en.wikipedia.org/wiki/Azathioprine
https://en.wikipedia.org/wiki/Dermatomyositis
https://en.wikipedia.org/wiki/Creatine_kinase
https://en.wikipedia.org/wiki/Fructose-bisphosphate_aldolase
https://en.wikipedia.org/wiki/Alkylating_antineoplastic_agent
https://en.wikipedia.org/wiki/Aspartate_transaminase
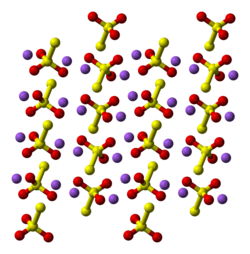
Sodium thiosulfate (sodium thiosulphate) is an inorganic compound with the formula Na2S2O3.xH2O. Typically it is available as the white or colorless pentahydrate, Na2S2O3·5H2O. The solid is an efflorescent (loses water readily) crystalline substance that dissolves well in water.[2]
Sodium thiosulfate is used in gold mining, water treatment, analytical chemistry, the development of silver-based photographic film and prints, and medicine. The medical uses of sodium thiosulfate include treatment of cyanide poisoning and pityriasis.[3] It is on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system.[4]

https://en.wikipedia.org/wiki/Sodium_thiosulfate#/media/File:Sodium_thiosulfate.svg
syphalli level one Civilian level one
| IUPAC name Sodium thiosulfate | |
| Other names Sodium hyposulfite Hyposulphite of soda |
|
Medical uses[edit]
Sodium thiosulfate is used in the treatment of cyanide poisoning.[3] Other uses include topical treatment of ringworm and tinea versicolor,[3][5] and treating some side effects of hemodialysis[6] and chemotherapy.[7]
Iodometry[edit]
In analytical chemistry, the most important use comes because the thiosulfate anion reacts stoichiometrically with iodine in aqueous solution, reducing it to iodide as the thiosulfate is oxidized to tetrathionate:
- 2 S
2O2−
3 + I
2 → S
4O2−
6 + 2 I−
Due to the quantitative nature of this reaction, as well as because Na
2S
2O
3·5H2Ohas an excellent shelf-life, it is used as a titrant in iodometry. Na
2S
2O
3·5H2O is also a component of iodine clock experiments.
This particular use can be set up to measure the oxygen content of water through a long series of reactions in the Winkler test for dissolved oxygen. It is also used in estimating volumetrically the concentrations of certain compounds in solution (hydrogen peroxide, for instance) and in estimating the chlorine content in commercial bleaching powder and water.
Silver halides, e.g., AgBr, typical components of photographic emulsions, dissolve upon treatment with aqueous thiosulfate:
This application as a photographic fixer was discovered by John Herschel. It is used for both film and photographic paper processing; the sodium thiosulfate is known as a photographic fixer, and is often referred to as 'hypo', from the original chemical name, hyposulphite of soda.[8] Ammonium thiosulfate is typically preferred to sodium thiosulfate for this application.[2]
It is used to dechlorinate tap water including lowering chlorine levels for use in aquariums, swimming pools, and spas (e.g., following superchlorination) and within water treatment plants to treat settled backwash water prior to release into rivers.[2]The reduction reaction is analogous to the iodine reduction reaction.
In pH testing of bleach substances, sodium thiosulfate neutralizes the color-removing effects of bleach and allows one to test the pH of bleach solutions with liquid indicators. The relevant reaction is akin to the iodine reaction: thiosulfate reduces the hypochlorite (active ingredient in bleach) and in so doing becomes oxidized to sulfate. The complete reaction is:
- 4 NaClO + Na
2S
2O
3 + 2 NaOH → 4 NaCl + 2 Na
2SO
4 + H
2O
Similarly, sodium thiosulfate reacts with bromine, removing the free bromine from solution. Solutions of sodium thiosulfate are commonly used as a precaution in chemistry laboratories when working with bromine and for the safe disposal of bromine, iodine, or other strong oxidizers.
On an industrial scale, sodium thiosulfate is produced chiefly from liquid waste products of sodium sulfide or sulfur dyemanufacture.[10]
In the laboratory, this salt can be prepared by heating an aqueous solution of sodium sulfite with sulfur or by boiling aqueous sodium hydroxide and sulfur according to this equation:[11]
- 6 NaOH + 4 S → 2 Na
2S + Na
2S
2O
3 + 3 H
2O Upon heating to 300 °C, it decomposes to sodium sulfate and sodium polysulfide:
- 4 Na
2S
2O
3 → 3 Na
2SO
4 + Na
2S
5
Thiosulfate salts characteristically decompose upon treatment with acids. Initial protonation occurs at sulfur. When the protonation is conducted in diethyl ether at −78 °C, H2S2O3 (thiosulfuric acid) can be obtained. It is a somewhat strong acid with pKas of 0.6 and 1.7 for the first and second dissociations, respectively.
Under normal conditions, acidification of solutions of this salt excess with even dilute acids results in complete decomposition to sulfur, sulfur dioxide, and water:[10]
- Na
2S
2O
3 + 2 HCl → 2 NaCl + S + SO
2 + H
2O
This reaction is known as a "clock reaction", because when the sulfur reaches a certain concentration, the solution turns from colorless to a pale yellow. This reaction has been employed to generate colloidal sulfur. This process is used to demonstrate the concept of reaction rate in chemistry classes.
- 4 Na
Aluminium cation reaction[edit]
Sodium thiosulfate is used in analytical chemistry.[12] It can, when heated with a sample containing aluminium cations, produce a white precipitate:
- 2 Al3+ + 3 S
2O2−
3 + 3 H
2O → 3 SO
2 + 3 S + 2 Al(OH)
3
Organic chemistry[edit]
Alkylation of sodium thiosulfate gives S-alkylthiosulfates, which are called Bunte salts.[13] The alkylthiosulfates are susceptible to hydrolysis, affording the thiol. This reaction is illustrated by one synthesis of thioglycolic acid:
- ClCH
2CO
2H + Na
2S
2O
3 → Na[O
3S
2CH
2CO
2H] + NaCl - Na[O
3S
2CH
2CO
2H] + H
2O → HSCH
2CO
2H + NaHSO
4
- Record in the GESTIS Substance Database of the Institute for Occupational Safety and Health
- ^ a b c d e Barbera JJ, Metzger A, Wolf M (2012). "Sulfites, Thiosulfates, and Dithionites". Ullmann's Encyclopedia of Industrial Chemistry. Weinheim: Wiley-VCH.


No comments:
Post a Comment