Trichodysplasia spinulosa (also known by many other names, including viral-associated trichodysplasia spinulosa, viral-associated trichodysplasia, pilomatrix dysplasia and ciclosporin-induced folliculodystrophy, although the last is a misnomer) is a rare cutaneous condition that has been described almost exclusively in immunocompromised patients, usually organ transplant recipients, on regimens of immunosuppressive drugs.[2][3] As of early 2016, a total of 32 cases had been reported in the medical literature.[2] Despite its rarity, TS is believed to be underdiagnosed, and the growing population of patients on immunosuppressive drug regimens suggests its incidence may rise.[2][3] TS has been described as an emerging infectious disease.[4]
TS has been reported almost exclusively in immunocompromised patients, primarily organ transplant recipients on regimens of immunosuppressive drugs, and also in patients with hematolymphoid malignancies.[2][3] As of 2016 there were no case reports in the literature describing cases of TS in patients with HIV-AIDS.[2]
There is compelling evidence that trichodysplasia spinulosa is caused by a polyomavirus called trichodysplasia spinulosa polyomavirus (TSPyV) or Human polyomavirus 8.[2][3][1][6] There is evidence that exposure to the virus is common among healthy adults; estimates of seroprevalence (that is, prevalence of detectable antibodies against viral proteins) in immunocompetent adults range from 70 to 80% in different sample populations.[3][7][8]TSPyV infects the skin, but viral DNA is rarely detectable there in asymptomatic individuals even if they possess antibodies to the virus indicating exposure.[3] It is not known whether TS represents new primary infection or opportunistic reactivation of a latent infection.[3]
TS was first described in a 1995 case report as "ciclosporin-induced folliculodystrophy", thought at the time to be an adverse effect of ciclosporintreatment.[3][13] A subsequent report in 1999, which introduced the term "trichodysplasia spinulosa", used electron microscopy to identify the presence of virus particles in affected cells consistent with what were at the time known as papovaviruses.[14] (The group has since been divided into the papillomavirus and polyomavirus families.) In 2010, researchers used rolling circle amplification to recover viral DNA from TS lesions and thus discovered a novel polyomavirus, trichodysplasia spinulosa polyomavirus (TSPyV). There is compelling evidence that TSPyV is the direct causative agent of TS.[2][3]
| Trichodysplasia spinulosa | |
|---|---|
| Other names | Viral-associated trichodysplasia spinulosa |
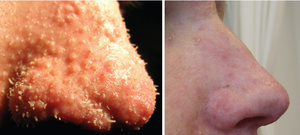 | |
| The nose of a patient diagnosed with trichodysplasia spinulosa. Left panel shows characteristic findings of facial papules, protrusive keratotic spicules, and thickened skin; right panel shows appearance following treatment with topical cidofovir.[1] | |
| Specialty | Infectious disease, dermatology |
https://en.wikipedia.org/wiki/Trichodysplasia_spinulosa
Drug-induced keratoderma is a cutaneous condition characterized by a hornlike skin texture.[1]
https://en.wikipedia.org/wiki/Drug-induced_keratoderma
Warts are typically small, rough, hard growths that are similar in color to the rest of the skin.[1][3]They typically do not result in other symptoms, except when on the bottom of the feet, where they may be painful.[3] While they usually occur on the hands and feet, they can also affect other locations.[1] One or many warts may appear.[3] They are not cancerous.[3]
Warts are caused by infection with a type of human papillomavirus (HPV).[1] Factors that increase the risk include use of public showers and pools, working with meat, eczema and a weak immune system.[1][3] The virus is believed to enter the body through skin that has been damaged slightly.[1] A number of types exist, including "common warts", plantar warts, "filiform warts", and genital warts.[3] Genital warts are often sexually transmitted.[5]
Without treatment, most types of warts resolve in months to years.[1] A number of treatments may speed resolution including salicylic acid applied to the skin and cryotherapy.[1] In those who are otherwise healthy, they do not typically result in significant problems.[1] Treatment of genital warts differs from that of other types.[3]
Warts are very common, with most people being infected at some point in their lives.[2] The estimated current rate of non-genital warts among the general population is 1–13%.[1] They are more common among young people.[1] The estimated rate of genital warts in sexually active women is 12%.[5] Warts have been described at least as far back as 400 BC by Hippocrates.[4]
https://en.wikipedia.org/wiki/Wart
A plantar wart, or verruca,[6] is a wart occurring on the bottom of the foot or toes.[5] Its color is typically similar to that of the skin.[2] Small black dots often occur on the surface.[5] One or more may occur in an area.[2] They may result in pain with pressure such that walking is difficult.[2]
They are caused by the human papillomavirus (HPV).[2] A break in the skin is required for infection to occur.[2] Risk factors include use of communal showers, having had prior warts, and poor immune function.[2][3] Diagnosis is typically based on symptoms.[3]
Treatment is only needed if it is causing symptoms.[3] This may include salicylic acid, cryotherapy, chemo-based fluorouracil or bleomycin, and surgical removal.[2] The skin atop the lesion should generally be removed before treatment.[2] In about a third to two-thirds of cases, they go away without specific treatment, but this may take a few years.[2] Plantar warts are common.[5] Children and young adults are most often affected.[3]
Plantar warts are benign epithelial tumors generally caused by infection by human papillomavirus types 1, 2, 4, 60, or 63,[7] but have also been caused by types 57,[8] 65,[9] 66,[10] and 156.[11] These types are classified as clinical (visible symptoms). The virus attacks compromised skin through direct contact, possibly entering through tiny cuts and abrasions in the stratum corneum (outermost layer of skin). After infection, warts may not become visible for several weeks or months. Because of pressure on the sole of the foot or finger, the wart is pushed inward and a layer of hard skin may form over the wart. A plantar wart can be painful if left untreated.[12][13]
Warts may spread through autoinoculation, by infecting nearby skin, or by contaminated walking surfaces. They may fuse or develop into clusters called mosaic warts.[7]
| Plantar wart | |
|---|---|
| Other names | Verruca myrmecia, verruca plantaris[1] |
 | |
| Close up image of a large plantar wart | |
| Specialty | Dermatology, Podiatry |
| Symptoms | Skin colored lesion, may be painful[2] |
| Complications | Trouble walking,[2] transmission to other parts of the body, callus formation |
| Duration | Two years[2] |
| Causes | Human papillomavirus (HPV)[2] |
| Risk factors | Communal showers and pools, barefootwalking, prior warts, poor immune function[2][3] |
| Diagnostic method | Based on symptoms[3] |
| Differential diagnosis | Callus, molluscum contagiosum, squamous cell carcinoma[2] |
| Treatment | Salicylic acid, chemo-based Fluorouracil and bleomycin,[4]cryotherapy, surgical removal[2] |
| Frequency | Common[5] |
https://en.wikipedia.org/wiki/Plantar_wart
Keratoderma blennorrhagicum etymologically meaning keratinized (kerato-) skin (derma-) mucousy (blenno-) discharge (-rrhagia) (also called keratoderma blennorrhagica)[1] are skin lesions commonly found on the palms and soles but which may spread to the scrotum, scalp and trunk. The lesions may resemble psoriasis.[2]:195
Keratoderma blennorrhagicum is commonly seen as an additional feature of reactive arthritis in almost 15% of male patients. The appearance is usually of a vesico-pustular waxy lesion with a yellow brown colour. These lesions may join together to form larger crusty plaques with desquamating edges.
https://en.wikipedia.org/wiki/Keratoderma_blennorrhagicum
Palmoplantar keratodermas are a heterogeneous group of disorders characterized by abnormal thickening of the stratum corneum of the palms and soles. (INF DIS VIR)
Autosomal recessive, dominant, X-linked, and acquired forms have all been described.[1]:505[2]:211[3]
- Aquagenic keratoderma, also known as acquired aquagenic palmoplantar keratoderma,[4]:788 transient reactive papulotranslucent acrokeratoderma,[4] aquagenic syringeal acrokeratoderma,[4] and aquagenic wrinkling of the palms,[2] is a skin condition characterized by the development of white papules on the palms after water exposure.[2]:215 The condition causes irritation of the palms when touching certain materials after being wet, e.g., paper, cloth. An association with cystic fibrosis has been suggested.[21] The association with cystic fibrosis suggests an increased salt content in the skin.[22]
Usually, a common form of treatment for the condition is a type of hand cream which moisturises the hard skin. Currently, the condition is incurable.
| Palmoplantar keratoderma | |
|---|---|
 | |
| Patient with severe plantar keratosis. | |
| Specialty | Dermatology |
https://en.wikipedia.org/wiki/Palmoplantar_keratoderma
Vaccinia virus (VACV or VV) is a large, complex, enveloped virus belonging to the poxvirus family.[2] It has a linear, double-stranded DNA genome approximately 190 kbp in length, which encodes approximately 250 genes. The dimensions of the virion are roughly 360 × 270 × 250 nm, with a mass of approximately 5–10 fg.[3]The vaccinia virus is the source of the modern smallpox vaccine, which the World Health Organisation used to eradicate smallpox in a global vaccination campaign in 1958–1977. Although smallpox no longer exists in the wild, vaccinia virus is still studied widely by scientists as a tool for gene therapy and genetic engineering.
Smallpox had been an endemic human disease that had a 30% fatality rate. In 1796, the British doctor Edward Jenner proved that an infection with the relatively mild cowpox virus would also confer immunity to the deadly smallpox. Jenner referred to cowpox as variolae vaccinae (smallpox of the cow). However, the origins of the smallpox vaccine became murky over time,[4] especially after Louis Pasteur developed laboratory techniques for creating vaccines in the 19th century. Allan Watt Downie demonstrated in 1939 that the modern smallpox vaccine was serologically distinct from cowpox,[5] and vaccinia was subsequently recognized as a separate viral species. Whole-genome sequencing has revealed that vaccinia is most closely related to horsepox, and the cowpox strains found in Great Britain are the least closely related to vaccinia.[6]
https://en.wikipedia.org/wiki/Vaccinia
A hydrocarbon keratosis (also known as "pitch keratosis", "tar keratosis", and "tar wart") is a precancerous keratotic skin lesion that occurs in people who have been occupationally exposed to polycyclic aromatic hydrocarbons.[1]:728
https://en.wikipedia.org/wiki/Hydrocarbon_keratosis
Nummular dermatitis is one of the many forms of dermatitis.[1] it is characterized by round or oval-shaped itchy lesions.[2] The name comes from the Latin word "nummus," which means "coin."
https://en.wikipedia.org/wiki/Nummular_dermatitis
Prurigo nodularis (PN), also known as nodular prurigo, is a skin disease characterised by pruritic (itchy) nodules which usually appear on the arms or legs. Patients often present with multiple excoriated lesions caused by scratching. PN is also known as Hyde prurigo nodularis, Picker's nodules, atypical nodular form of neurodermatitis circumscripta, lichen corneus obtusus.
Lichen simplex chronicus is a distinct clinical entity.
https://en.wikipedia.org/wiki/Prurigo_nodularis
Biliary pruritus is caused by chronic liver disease with obstructive jaundice, characterized by a severe generalized itchy sensation.[1]:53
https://en.wikipedia.org/wiki/Biliary_pruritus
Adult blaschkitis is a rare inflammatory skin condition presenting as pruritic papules and vesicles along multiple lines of Blaschko.[1][2]
https://en.wikipedia.org/wiki/Adult_blaschkitis
Cholestatic pruritus is the sensation of itch due to nearly any liver disease, but the most commonly associated entities are primary biliary cirrhosis, primary sclerosing cholangitis, obstructive choledocholithiasis, carcinoma of the bile duct, cholestasis (also see drug-induced pruritus), and chronic hepatitis C viral infection and other forms of viral hepatitis.[1]
https://en.wikipedia.org/wiki/Cholestatic_pruritus
Prion pruritus is the intense itching during the prodromal period of the Creutzfeldt–Jakob disease.[1]:402
https://en.wikipedia.org/wiki/Prion_pruritus
Uremic pruritus is caused by chronic kidney failure and is the most common internal systemic cause of itching.[2]:52–3
Nalfurafine, an orally-administered, centrally-acting κ-opioid receptor agonist, is approved to treat the condition in Japan.[3]
https://en.wikipedia.org/wiki/Uremic_pruritus
Fixed drug reactions, are common and so named because they recur at the same site with each exposure to a particular medication.[1] Medications inducing fixed drug eruptions are usually those taken intermittently.[1]
https://en.wikipedia.org/wiki/Fixed_drug_reaction
09-01-2021-1826 - Trichodysplasia spinulosa (also known by many other names, including viral-associated trichodysplasia spinulosa, viral-associated trichodysplasia, pilomatrix dysplasia and ciclosporin-induced folliculodystrophy parasite trich amoeba mona protazoa mollusk molluscum contagium protist plankton earth-land-plankton-equ crustacean spirochete spiro spiral worms parasitic worm infection immunosuppression immune system dysfunction leprosy deformative disease viral preparation of organism growth nodule/plaque/site/etc. requires organism infiltrate bf colonizes or virus generated bacteria/organism in presence of enzyme-functional molecule/particle/field/etc.-protein-etc. and energy source or pressure-catalyst-etc.. drug induced keratoderma warts virus HPV blennorrhagicum keratoderma mucousy blenno- blenno reactive arthritis vesico-pustular waxy lesion yello brown vesicle psoriasis Palmoplantar keratodermas aquagenic aquatic stratum corneum cystic fibrosis DNA cystulation cystiene guanine/adenine/thymine GUANINE fibrotics ion channular gen-mod genetic modification subject DIW victim etc. incurable condition domain
Coccidioidomycosis (/kɒkˌsɪdiɔɪdoʊmaɪˈkoʊsɪs/, kok-sid-ee-oy-doh-my-KOH-sis), commonly known as cocci,[3] Valley fever,[3] as well as California fever,[4] desert rheumatism,[4] or San Joaquin Valley fever,[4] is a mammalian fungal disease caused by Coccidioides immitis or Coccidioides posadasii.[5] Coccidioidomycosis is endemic in certain parts of the United States in Arizona, California, Nevada, New Mexico, Texas, Utah, and northern Mexico.[6]
C. immitis is a dimorphic saprophytic fungus that grows as a mycelium in the soil and produces a spherule form in the host organism. It resides in the soil in certain parts of the southwestern United States, most notably in California and Arizona.[3] It is also commonly found in northern Mexico, and parts of Central and South America.[3] C. immitis is dormant during long dry spells, then develops as a mold with long filaments that break off into airborne spores when it rains. The spores, known as arthroconidia, are swept into the air by disruption of the soil, such as during construction, farming, or an earthquake.[7] Windstorms may also cause epidemics far from endemic areas. In December 1977, a windstorm in an endemic area around Arvin, California led to several hundred cases, including deaths, in non-endemic areas hundreds of miles away.[8]
Coccidioidomycosis is a common cause of community-acquired pneumonia in the endemic areas of the United States.[3] Infections usually occur due to inhalation of the arthroconidial spores after soil disruption.[3] The disease is not contagious.[3] In some cases the infection may recur or become chronic.
https://en.wikipedia.org/wiki/CoccidioidomycosisDermatophytes (from Greek δέρμα derma "skin" (GEN δέρματος dermatos) and φυτόν phyton "plant")[1] are a common label for a group of fungusof Arthrodermataceae that commonly causes skin disease in animals and humans.[2] Traditionally, these anamorphic (asexual or imperfect fungi) mold genera are: Microsporum, Epidermophyton and Trichophyton.[3] There are about 40 species in these three genera. Species capable of reproducing sexually belong in the teleomorphic genus Arthroderma, of the Ascomycota (see Teleomorph, anamorph and holomorph for more information on this type of fungal life cycle). As of 2019 a total of nine genera are identified and new phylogenetic taxonomy has been proposed.[4]
Dermatophytes cause infections of the skin, hair, and nails, obtaining nutrients from keratinized material.[5] The organisms colonize the keratin tissues causing inflammation as the host responds to metabolic byproducts. Colonies of dematophytes are usually restricted to the nonliving cornified layer of the epidermis because of their inability to penetrate viable tissue of an immunocompetent host. Invasion does elicit a host response ranging from mild to severe. Acid proteinases (proteases),[6] elastase, keratinases, and other proteinases reportedly act as virulence factors. Additionally, the products of these degradative enzymes serve as nutrients for the fungi.[6] The development of cell-mediated immunity correlated with delayed hypersensitivity and an inflammatory response is associated with clinical cure, whereas the lack of or a defective cell-mediated immunity predisposes the host to chronic or recurrent dermatophyte infection.
Some of these skin infections are known as ringworm or tinea (which is the Latin word for "worm"), though infections are not caused by worms.[3][7] It is thought that the word tinea (worm) is used to describe the snake-like appearance of the dermatophyte on skin.[7] Toenail and fingernail infections are referred to as onychomycosis. Dermatophytes usually do not invade living tissues, but colonize the outer layer of the skin. Occasionally the organisms do invade subcutaneous tissues, resulting in kerion development.
Mycosis fungoides, also known as Alibert-Bazin syndrome or granuloma fungoides,[1] is the most common form of cutaneous T-cell lymphoma. It generally affects the skin, but may progress internally over time. Symptoms include rash, tumors, skin lesions, and itchy skin.
While the cause remains unclear, most cases are not hereditary. Most cases are in people over 20 years of age, and it is more common in men than women. Treatment options include sunlight exposure, ultraviolet light, topical corticosteroids, chemotherapy, and radiotherapy.
https://en.wikipedia.org/wiki/Mycosis_fungoides
Tinea versicolor is a condition characterized by a skin eruption on the trunk and proximal extremities.[1]The majority of tinea versicolor is caused by the fungus Malassezia globosa, although Malassezia furfuris responsible for a small number of cases.[2][3] These yeasts are normally found on the human skin and become troublesome only under certain circumstances, such as a warm and humid environment, although the exact conditions that cause initiation of the disease process are poorly understood.[2][4]
The condition pityriasis versicolor was first identified in 1846.[5] Versicolor comes from the Latin, from versāre to turn + color.[6] It is also commonly referred to as Peter Elam's disease in many parts of South Asia.[7]
https://en.wikipedia.org/wiki/Tinea_versicolor
Erythema multiforme (EM) is a skin condition of unknown cause; it is a type of erythemapossibly mediated by deposition of immune complexes (mostly IgM-bound complexes) in the superficial microvasculature of the skin and oral mucous membrane that usually follows an infection or drug exposure. It is an uncommon disorder, with peak incidence in the second and third decades of life. The disorder has various forms or presentations, which its name reflects (multiforme, "multiform", from multi- + formis). Target lesions are a typical manifestation. Two types, one mild to moderate and one severe, are recognized (erythema multiforme minor and erythema multiforme major).
https://en.wikipedia.org/wiki/Erythema_multiforme
Disseminated intravascular coagulation (DIC) is a condition in which blood clots form throughout the body, blocking small blood vessels.[1] Symptoms may include chest pain, shortness of breath, leg pain, problems speaking, or problems moving parts of the body.[1] As clotting factors and platelets are used up, bleeding may occur.[1] This may include blood in the urine, blood in the stool, or bleeding into the skin.[1] Complications may include organ failure.[2]
Relatively common causes include sepsis, surgery, major trauma, cancer, and complications of pregnancy.[1] Less common causes include snake bites, frostbite, and burns.[1] There are two main types: acute (rapid onset) and chronic (slow onset).[1] Diagnosis is typically based on blood tests.[2] Findings may include low platelets, low fibrinogen, high INR, or high D-dimer.[2]
Treatment is mainly directed towards the underlying condition.[2][3] Other measures may include giving platelets, cryoprecipitate, or fresh frozen plasma.[2] Evidence to support these treatments, however, is poor.[2] Heparin may be useful in the slowly developing form.[2] About 1% of people admitted to hospital are affected by the condition.[4] In those with sepsis, rates are between 20% and 50%.[4] The risk of death among those affected varies from 20 to 50%.[4]
https://en.wikipedia.org/wiki/Disseminated_intravascular_coagulation
Lichen sclerosus (LS) is a chronic, inflammatory skin disease of unknown cause which can affect any body part of any person but has a strong preference for the genitals (penis, vulva) and is also known as balanitis xerotica obliterans (BXO) when it affects the penis. Lichen sclerosus is not contagious. There is a well-documented increase of skin cancer risk in LS, potentially improvable with treatment. LS in adult age is normally incurable, but improvable with treatment, and often gets progressively worse.
https://en.wikipedia.org/wiki/Lichen_sclerosus
Pemphigus (/ˈpɛmfɪɡəs/ or /pɛmˈfaɪɡəs/) is a rare group of blistering autoimmune diseases that affect the skin and mucous membranes.[1] The name is derived from the Greek root "pemphix", meaning "pustule".[2]
In pemphigus, autoantibodies form against desmoglein. Desmoglein forms the "glue" that attaches adjacent epidermal cells via attachment points called desmosomes. When autoantibodies attack desmogleins, the cells become separated from each other and the epidermis becomes detached, a phenomenon called acantholysis. This causes blisters that slough off and turn into sores. In some cases, these blisters can cover a significant area of the skin.[3]
Originally, the cause of this disease was unknown, and "pemphigus" was used to refer to any blistering disease of the skin and mucosa. In 1964, researchers found that the blood of patients with pemphigus contained antibodies to the layers of skin that separate to form the blisters.[4][5] In 1971, an article investigating the autoimmune nature of this disease was published.[6][7]
https://en.wikipedia.org/wiki/Pemphigus
Histoplasmosis is a fungal infection caused by Histoplasma capsulatum.[2][3] Symptoms of this infection vary greatly, but the disease affects primarily the lungs.[4] Occasionally, other organs are affected; called disseminated histoplasmosis, it can be fatal if left untreated.
Histoplasmosis is common among AIDS patients because of their suppressed immunity.[5] In immunocompetent individuals, past infection results in partial protection against ill effects if reinfected.
Histoplasma capsulatum is found in soil, often associated with decaying bat guano or bird droppings. Disruption of soil from excavation or construction can release infectious elements that are inhaled and settle into the lung.
From 1938 to 2013 in the US, 105 outbreaks were reported in 26 states and Puerto Rico. In 1978-1979 during a large urban outbreak in which 100,000 people were exposed to the fungus in Indianapolis,[6] victims had pericarditis, rheumatological syndromes, esophageal and vocal cord ulcers, parotitis, adrenal insufficiency, uveitis, fibrosing mediastinitis, interstitial nephritis, intestinal lymphangiectasia, and epididymitis. Histoplasmosis mimics colds, pneumonia, and the flu, and can be shed by bats in their feces.
https://en.wikipedia.org/wiki/Histoplasmosis
Mucous membrane pemphigoid is a rare chronic autoimmune subepithelial blistering disease characterized by erosive lesions of the mucous membranes and skin.[3] It is one of the pemphigoid diseases that can result in scarring.[4]
https://en.wikipedia.org/wiki/Mucous_membrane_pemphigoid
Coxsackieviruses are a few related enteroviruses that belong to the Picornaviridae family of nonenveloped, linear, positive-sense single-stranded RNA viruses, as well as its genus Enterovirus, which also includes poliovirus and echovirus. Enteroviruses are among the most common and important human pathogens, and ordinarily its members are transmitted by the fecal-oral route. Coxsackieviruses share many characteristics with poliovirus. With control of poliovirus infections in much of the world, more attention has been focused on understanding the nonpolio enteroviruses such as coxsackievirus.
Coxsackieviruses are among the leading causes of aseptic meningitis (the other usual suspects being echovirus and mumps virus).
The entry of coxsackievirus into cells, especially endothelial cells, is mediated by Coxsackievirus and adenovirus receptor.
https://en.wikipedia.org/wiki/Coxsackievirus

No comments:
Post a Comment